Peritoneal Dialysis
Comprehensive peritoneal dialysis guide for paramedics and nurses - principles, modalities, complications, and patient care.
Comprehensive peritoneal dialysis guide for paramedics and nurses - principles, modalities, complications, and patient care.
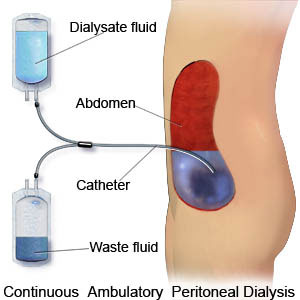
Peritoneal dialysis (PD) is a form of renal replacement therapy that uses the patient's own peritoneal membrane as the semipermeable "dialyzer" to remove waste products, correct electrolytes and acid-base disturbances, and remove excess fluid.
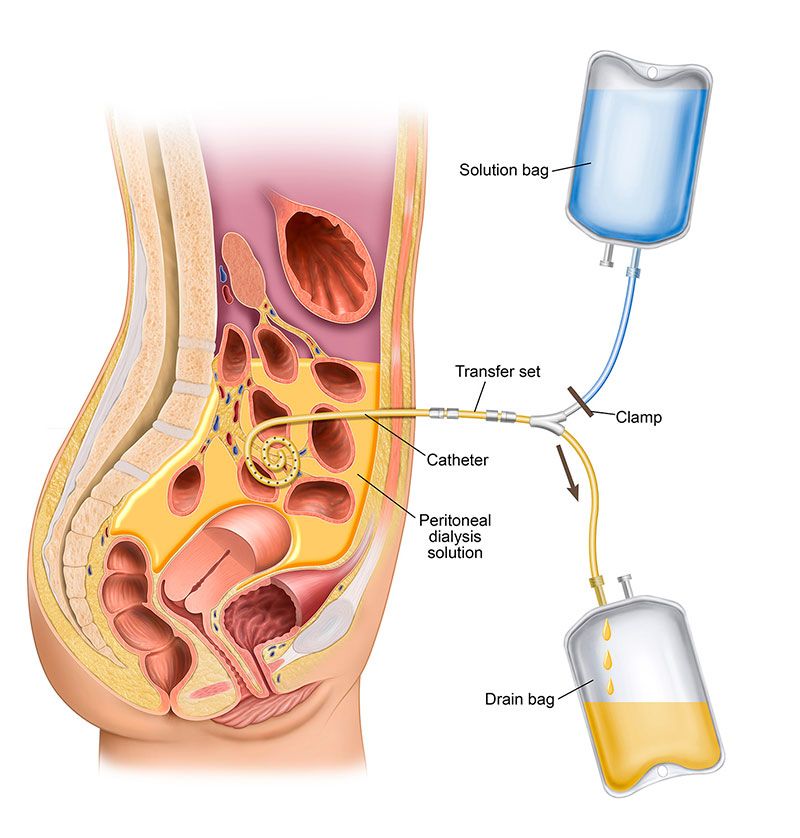
A soft catheter is placed into the peritoneal cavity. Sterile dialysis solution (dialysate) is infused into the abdomen, where it dwells in contact with the peritoneal capillary bed. Solutes and water move between blood and dialysate, and then the used fluid is drained out and replaced with fresh solution.
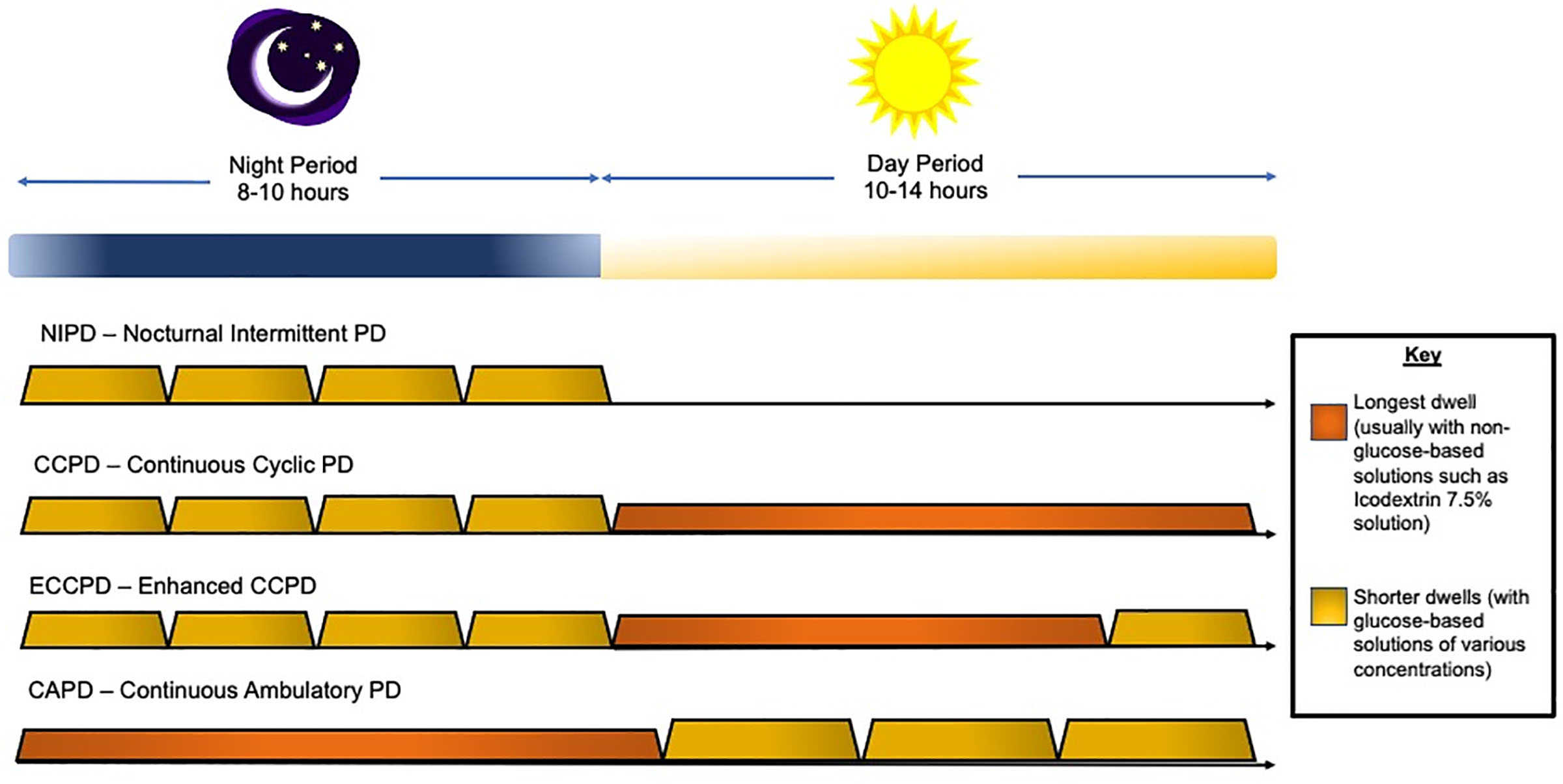
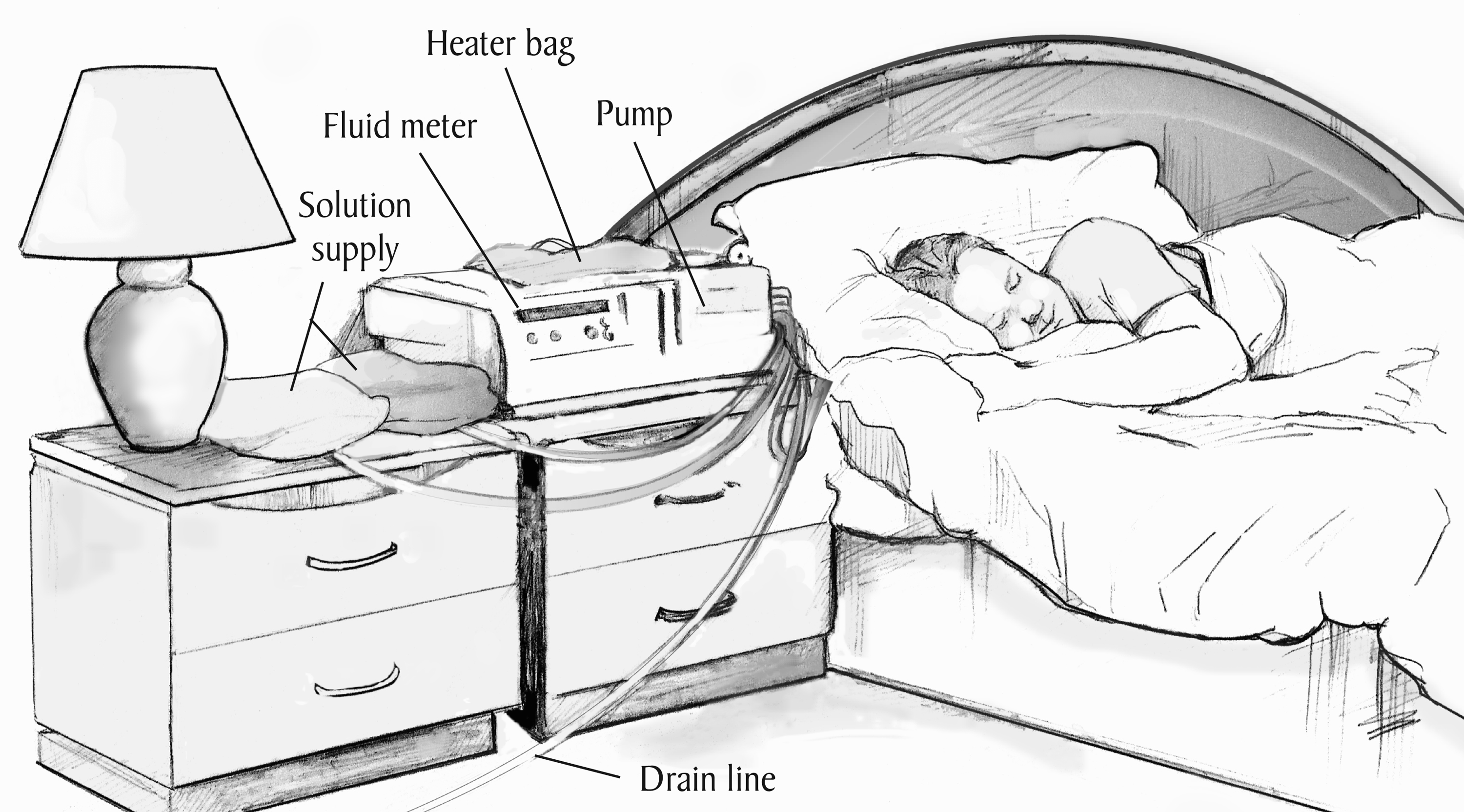
PD is most commonly a home-based therapy for patients with end-stage kidney disease (ESKD). It can be performed manually during the day (CAPD) or automatically at night using a cycler (APD). Nurses in acute and chronic settings support patient training, monitoring, troubleshooting, and infection prevention.
There are two main types of peritoneal dialysis used in practice:
Peritoneal dialysis is one of several options for long-term dialysis in ESKD. It may be chosen for:
Absolute or strong contraindications are uncommon but include situations where PD cannot function or would be unsafe.
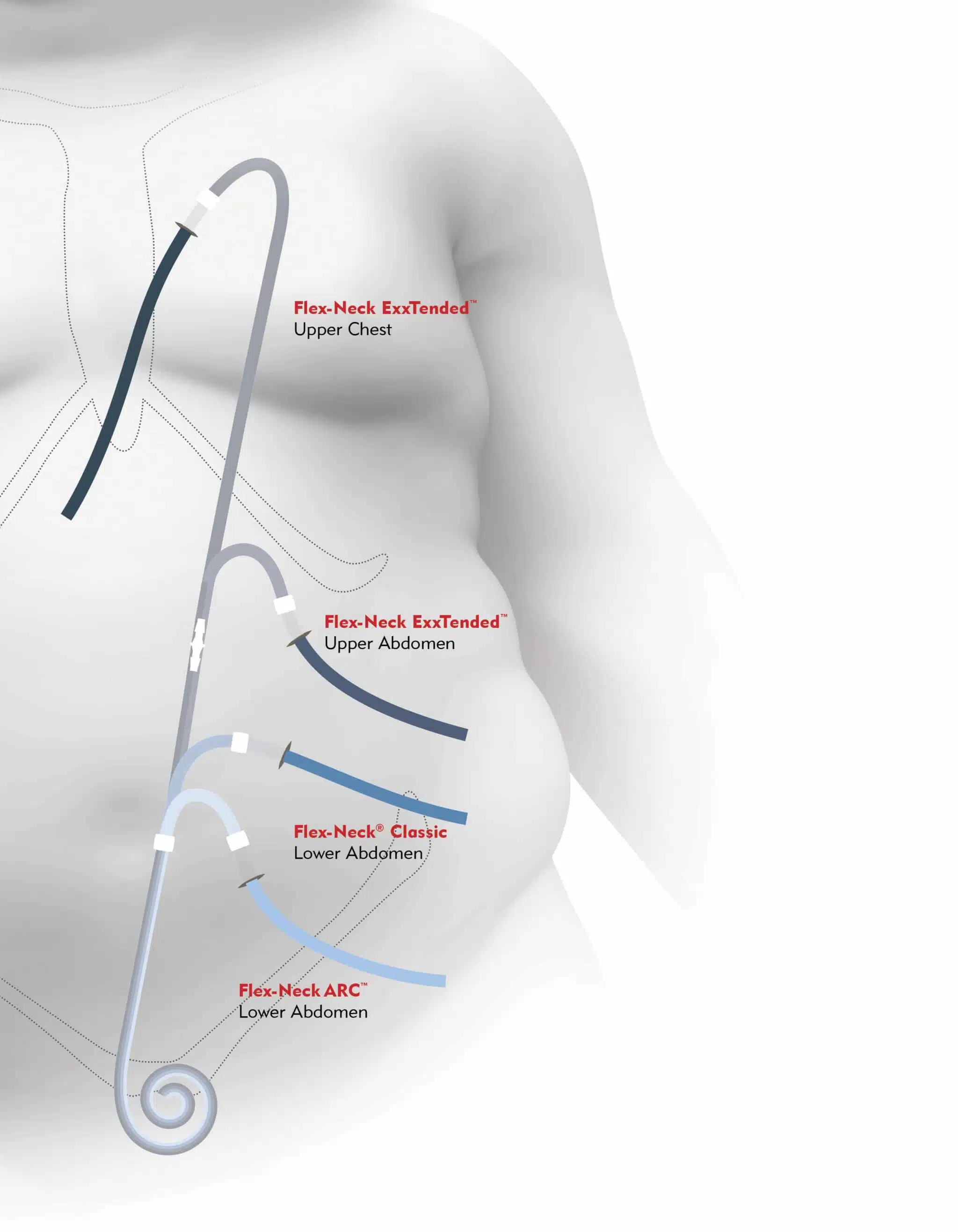
The PD catheter is a soft, flexible tube placed into the peritoneal cavity, usually via laparoscopic or open surgical technique.
PD works through diffusion and osmosis across the peritoneal membrane:
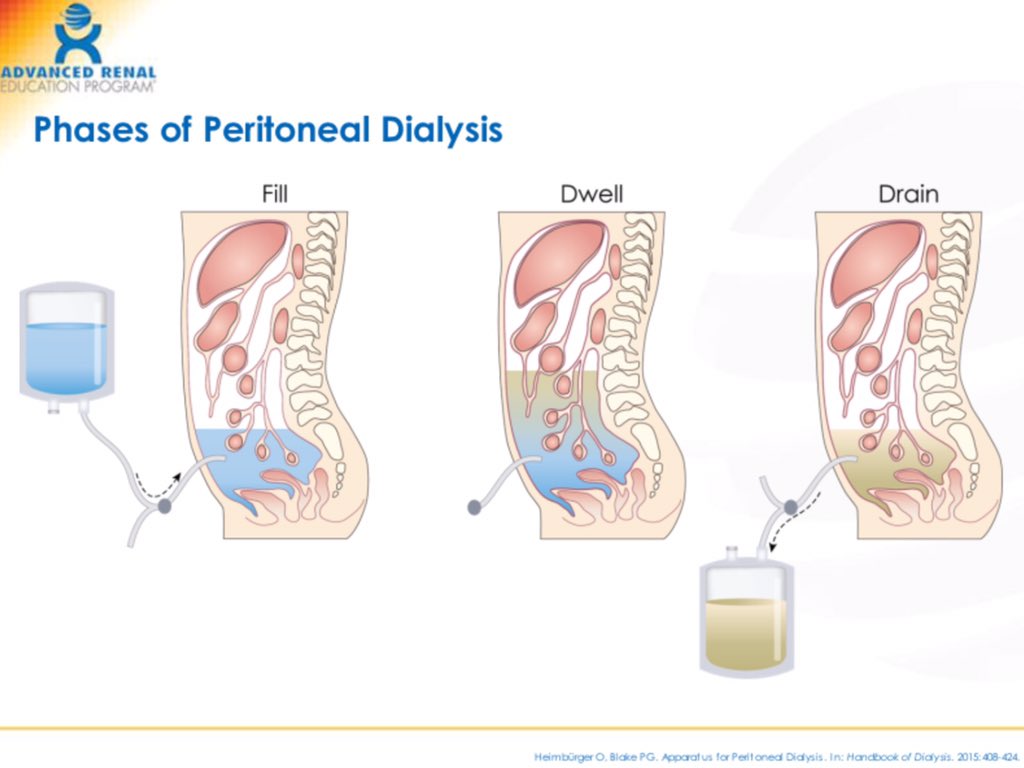
A typical CAPD exchange (manual PD) involves a structured, aseptic process. Details vary by system (Baxter, Fresenius, etc.), but the core steps are similar:
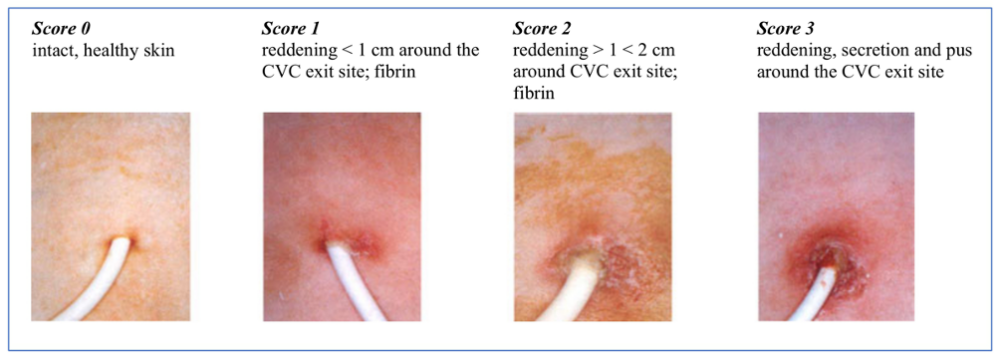
Key assessments for patients on PD (inpatient or outpatient visits):
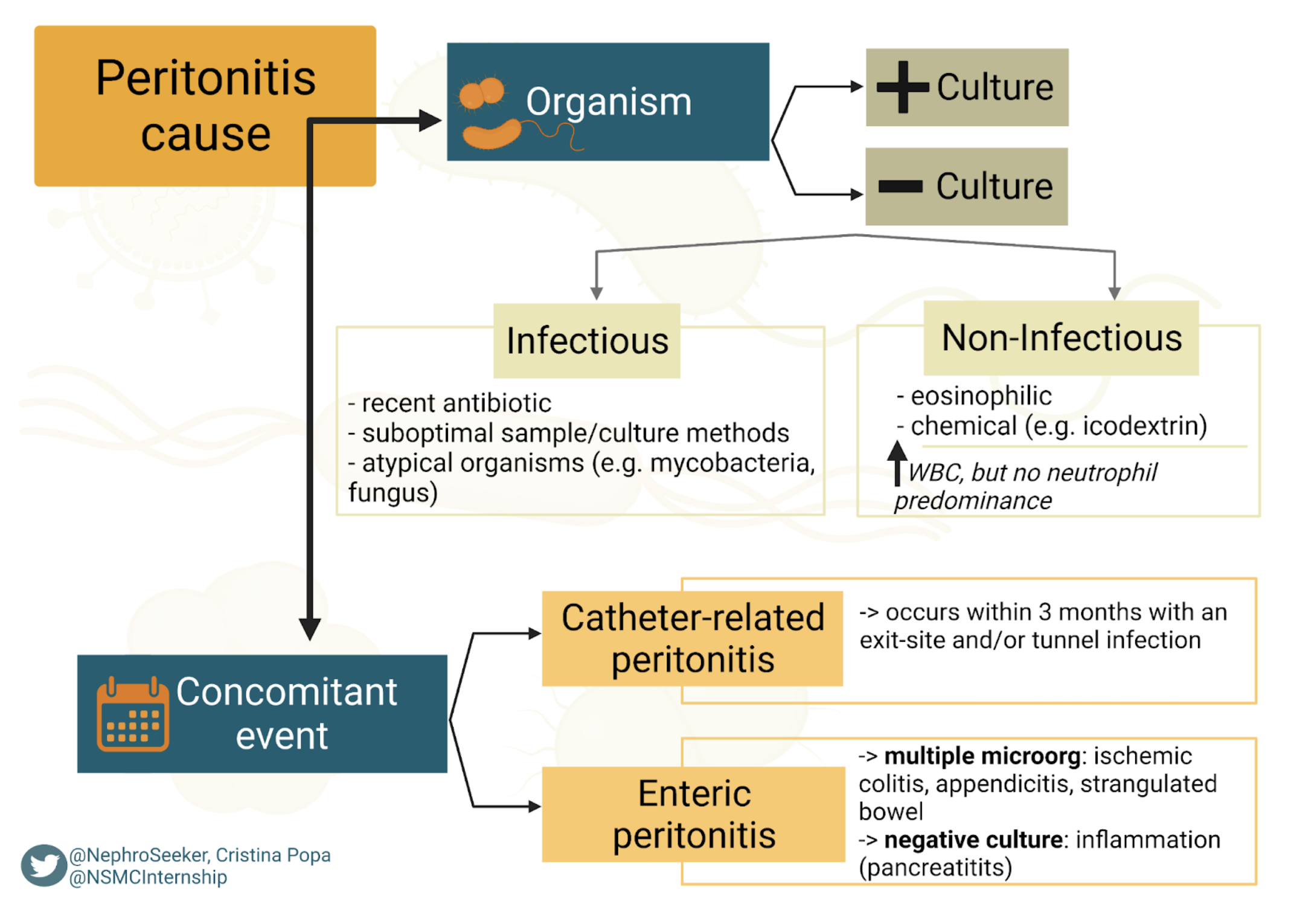
Nursing and patient practices that reduce infection risk:
Core teaching points for patients starting or maintaining PD: