Medical Disclaimer
- For Educational Purposes Only: This content is intended for educational reference and should not be used for clinical decision-making.
- Not a Substitute for Professional Judgment: Always consult your local protocols, institutional guidelines, and supervising physicians.
- Verify Before Acting: Users are responsible for verifying information through authoritative sources before any clinical application.
AI Assistance Notice
Bedside Snapshot
- Cardiac arrest
- Severe shock/trauma
- Failed IV access (2 attempts or 90 sec)
- Pediatric resuscitation
- Adult: Proximal humerus (fastest flow)
- Adult Alt: Proximal tibia
- Pediatric: Proximal tibia (preferred)
- Alt Sites: Distal tibia, distal femur
- EZ-IO power driver + needle set
- Extension tubing with Luer-lock
- 10mL flush syringe
- Pressure bag (for rapid infusion)
- Confirm placement: aspirate marrow
- Flush with 10mL saline
- 2% lidocaine 40mg for conscious patients
- Remove within 24 hours
Intraosseous (IO) access is an emergency vascular access technique that delivers fluids and medications directly into the bone marrow cavity. The bone marrow contains a rich network of venous sinusoids that drain directly into the central circulation, providing a reliable "non-collapsible" IV when peripheral veins are inaccessible.
Why IO Works
- Direct vascular access: Marrow sinusoids connect directly to central venous circulation
- Non-collapsible: Unlike veins, the bone marrow space doesn't collapse in shock
- Equivalent to IV: Drug absorption and onset times match intravenous delivery
- Rapid placement: Insertion takes 10-30 seconds with modern devices
Visualizing How IO Works
Historical Context
IO access was first described in 1922 and used extensively during World War II for battlefield resuscitation. After declining in favor of IV access, it experienced a renaissance in the 1980s with improved devices. Today, IO is considered equivalent to IV by AHA/ACLS guidelines and is the preferred alternative when IV access fails.
Emergency Indications
- Cardiac arrest – IO is first-line when IV not immediately available
- Severe shock – Hemorrhagic, septic, anaphylactic, or cardiogenic
- Major trauma – When peripheral veins are collapsed or inaccessible
- Severe dehydration – Especially in pediatric patients
- Status epilepticus – When IV access cannot be established
- Burns – When extremities are unavailable for peripheral access
Clinical Criteria for IO Use
- Failed IV attempts: 2 failed attempts OR 90 seconds without success
- Difficult access conditions: Obesity, edema, IV drug use history, vasculopathy
- Time-critical situations: When medication delivery cannot wait
What Can Be Administered via IO?
- All ACLS medications (epinephrine, amiodarone, lidocaine, etc.)
- Blood products (PRBCs, plasma, platelets)
- Crystalloid fluids (NS, LR)
- Vasopressors and inotropes
- Sedatives and analgesics
- Contrast media for CT imaging
- Antibiotics
Absolute Contraindications
- Fracture at insertion site – Fluid will extravasate through fracture
- Previous IO attempt in same bone (within 48 hours) – Risk of extravasation
- Overlying infection/cellulitis – Risk of osteomyelitis
- Prosthetic limb or joint at site
- Inability to identify landmarks
Relative Contraindications
- Osteoporosis – Increased risk of fracture, but not absolute
- Osteogenesis imperfecta – Brittle bone disease
- Osteopetrosis – Abnormally dense bone may prevent insertion
- Recent orthopedic surgery at the site
- Significant burns at insertion site
- Peripheral vascular disease – May affect perfusion
Site-Specific Contraindications
| Site | Avoid If... |
|---|---|
| Proximal Tibia | Knee surgery, tibial fracture, knee prosthesis |
| Proximal Humerus | Shoulder surgery, humeral fracture, rotator cuff repair |
| Distal Tibia | Ankle fracture, recent ankle surgery |
| Sternum (FAST1) | Sternotomy, chest trauma, CPR in progress |
Power-Driven: EZ-IO (Arrow/Teleflex)
The most widely used IO device in modern emergency medicine. Battery-powered driver with disposable needle sets.

EZ-IO Needle Sizes
| Needle | Color | Length | Patient Weight |
|---|---|---|---|
| Pediatric (PD) | Pink | 15mm | 3-39 kg |
| Adult (AD) | Blue | 25mm | ≥40 kg |
| Large Adult (LD) | Yellow | 45mm | ≥40 kg with excess tissue |
Spring-Loaded Devices

Bone Injection Gun (BIG)
- Disposable, single-use spring-loaded device
- Available in adult and pediatric sizes
- Set depth before insertion
- Pull safety, position, press trigger
FAST1 (First Access for Shock and Trauma)

- Designed specifically for sternal access in adults
- Multiple needle cluster penetrates manubrium
- Includes integrated target patch for landmark identification
- Not recommended during active CPR
Manual IO Needles
- Jamshidi needle – Most common manual needle
- Sur-Fast needle – Threaded design for stability
- Dieckmann needle – Shorter, designed for pediatrics
Manual needles require more force and technique. Best suited for pediatric patients with softer cortical bone. Less commonly used in adults due to dense cortex.
1. Proximal Humerus (Adult Preferred Site)
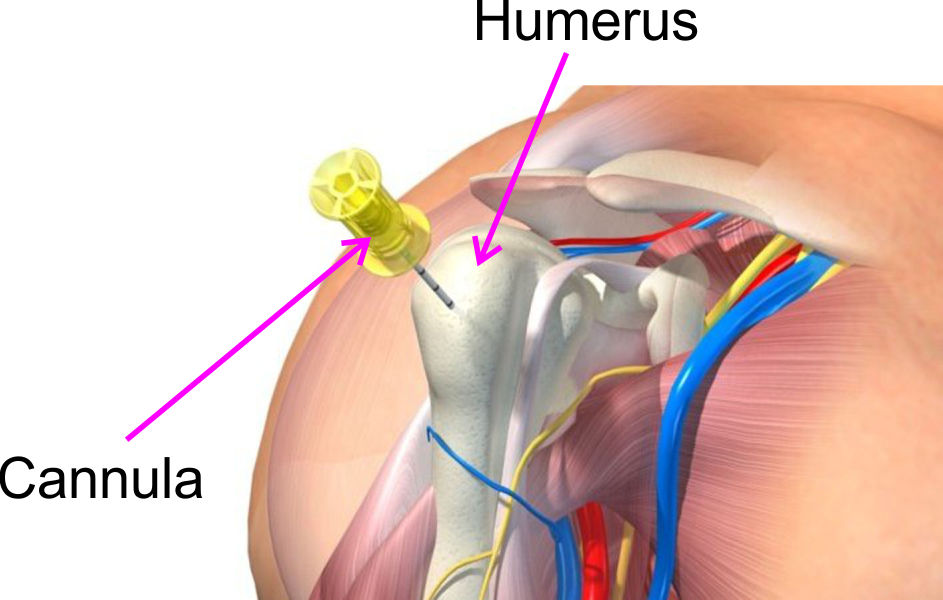
Landmarks
- Patient supine, arm adducted and internally rotated (hand on umbilicus)
- Palpate the greater tubercle – the bony prominence at the lateral shoulder
- Insertion site: 1-2 cm above the surgical neck
- Insert at 45° angle toward opposite hip
2. Proximal Tibia (Pediatric Preferred / Adult Alternative)
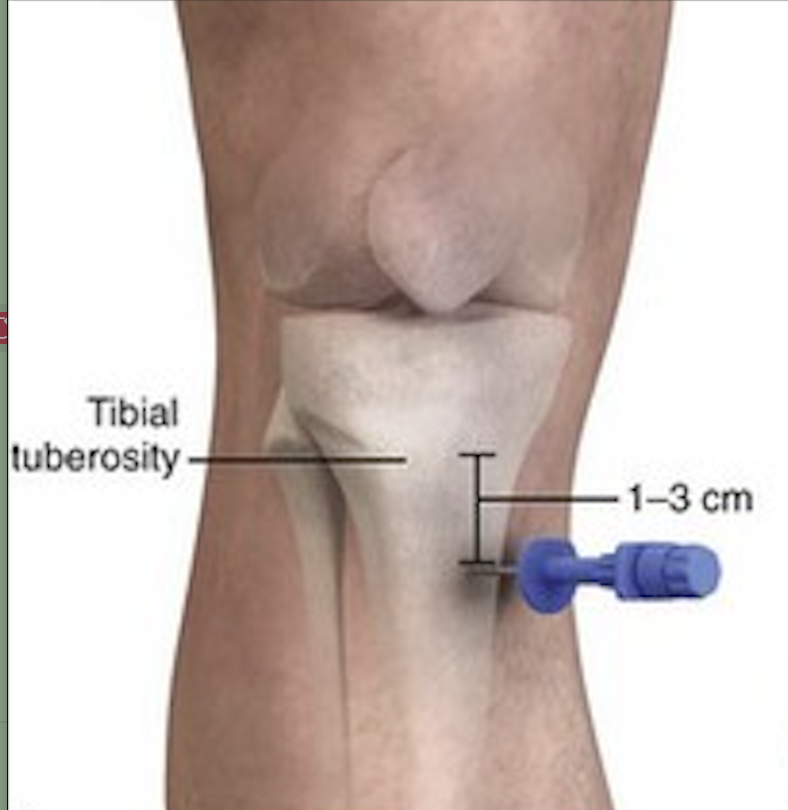
Landmarks
- Patient supine with knee slightly flexed (rolled towel under knee)
- Identify tibial tuberosity (bump below patella)
- Adult: 2 finger-breadths (2cm) below tuberosity, 1-2cm medial to tibial ridge
- Pediatric: 1 finger-breadth below tuberosity on flat anteromedial surface
- Insert at 90° to bone surface (perpendicular)
3. Distal Tibia

Landmarks
- Medial malleolus – the bony prominence at inner ankle
- Insertion site: 1-2cm proximal to medial malleolus
- Flat surface of distal tibial metaphysis
- Insert at 90° to bone surface
4. Distal Femur (Pediatric Alternative)

Landmarks
- Patient supine with knee slightly flexed
- Palpate patella and femoral condyles
- Insertion site: 1-2cm above patella on midline
- Insert at 10-15° angle toward head (into marrow cavity)
Site Selection Summary
| Site | Best For | Flow Rate | Notes |
|---|---|---|---|
| Proximal Humerus | Adults (1st choice) | ~5 L/hr | Fastest to central circulation |
| Proximal Tibia | Pediatrics (1st), Adults (2nd) | ~1-2 L/hr | Easiest landmarks, most studied |
| Distal Tibia | All ages (alternative) | ~1 L/hr | Easy access if knee inaccessible |
| Distal Femur | Pediatrics only | ~1 L/hr | Avoid growth plate in older children |
| Sternum | Adults (FAST1 only) | ~1-2 L/hr | Not during CPR; specialized device |
Pre-Procedure
- Confirm indication – Failed IV, cardiac arrest, critical patient
- Check contraindications – No fracture, no prior IO, no infection at site
- Select site – Proximal humerus (adult) or proximal tibia (pediatric)
- Select needle size – Based on patient weight and tissue depth
- Assemble equipment:
- EZ-IO driver with appropriate needle
- EZ-Stabilizer dressing
- Extension tubing with Luer-lock
- 10mL saline flush syringe
- 2% lidocaine (40mg) for conscious patients
- Pressure bag or infusion pump
EZ-IO Insertion Technique
- Position patient – Stabilize the limb; supine for most sites
- Clean insertion site – Antiseptic swab (chlorhexidine or alcohol)
- Stabilize the limb – Hold firmly but don't wrap hand around insertion site
- Remove safety cap from needle set
- Insert needle through skin to bone surface
- Proximal humerus: 45° angle toward opposite hip
- Tibia: 90° perpendicular to bone surface
- Confirm position – Needle should rest on bone, 5mm black line visible
- Squeeze trigger – Advance until hub reaches skin OR you feel "pop"
- Stop drilling when loss of resistance felt
- Stabilize hub and remove driver by pulling straight back
- Remove stylet by turning counterclockwise
Confirmation of Placement
- Needle stands upright without support
- Aspirate bone marrow – Dark, thick blood (may not always be present)
- Flush with 10mL saline – Should flow freely without resistance
- No extravasation – No swelling around site
Post-Insertion
- Apply EZ-Stabilizer or secure with tape
- Connect extension tubing with Luer-lock
- Lidocaine 2% – Slow push 20-40mg for conscious patients (wait 30-60 sec)
- Begin infusion – Pressure bag for bolus fluids
- Monitor site – Check for compartment syndrome signs
- Document – Time, site, needle size, confirmation methods
Flow Rate by Site (Under Pressure)
| Site | Gravity Flow | Pressure Bag (300mmHg) | Maximum Rate |
|---|---|---|---|
| Proximal Humerus | ~150 mL/hr | ~5000 mL/hr | ~5 L/hr |
| Proximal Tibia | ~75 mL/hr | ~1000-2000 mL/hr | ~2 L/hr |
| Distal Tibia | ~50 mL/hr | ~1000 mL/hr | ~1 L/hr |
| Sternum | ~100 mL/hr | ~1500 mL/hr | ~1.5 L/hr |
Optimizing Flow
- Pressure infusion – Always use 300mmHg pressure bag for bolus fluids
- Warm fluids – Cold fluids increase marrow resistance
- Prime with flush – Initial 10mL saline flush opens sinusoids
- Avoid air – Prime tubing completely; air embolism possible
Proximal Humerus Infusion Demonstration
Medication Administration
- Follow all medications with flush – 5-10mL saline push
- Drug onset equivalent to IV – No dose adjustment needed
- Vasopressors – Safe to administer; flush well after
- Blood products – Require pressure; may take longer but effective
Overall Complication Rate
IO access has a remarkably low complication rate (<1%) when performed correctly. Most complications are minor and related to technique errors that can be avoided with proper training.
Immediate Complications
| Complication | Cause | Prevention/Treatment |
|---|---|---|
| Extravasation | Through-and-through insertion, fracture, prior IO site | Remove needle, apply pressure, try alternate site |
| Infiltration | Needle dislodgement, incomplete insertion | Monitor infusion site, secure properly |
| Bone fracture | Excessive force, osteoporotic bone | Use powered driver, proper technique |
| Fat embolism | Marrow contents entering circulation | Rare; typically clinically insignificant |
| Pain during infusion | Marrow expansion from pressure | 2% lidocaine 40mg before infusion |
Delayed Complications
| Complication | Risk Factors | Prevention/Treatment |
|---|---|---|
| Osteomyelitis | Prolonged use (>24 hrs), contamination | Limit IO duration, sterile technique, remove promptly |
| Compartment syndrome | Extravasation into confined space | Monitor for pain, swelling, pallor; immediate fasciotomy if confirmed |
| Skin necrosis | Vasoconstrictor extravasation | Monitor site during vasopressor infusion |
| Growth plate injury | Improper insertion in children | Correct site selection on metaphysis |
Rare Complications
| Complication | Notes |
|---|---|
| Air embolism | Prime tubing completely before connection |
| Needle fracture | Very rare with modern devices |
| Injury to adjacent structures | Proper landmark identification prevents this |
Site Selection in Children
- Proximal tibia – First choice for all pediatric ages
- 1 finger-breadth below tibial tuberosity
- Flat anteromedial surface
- Insert 90° perpendicular to bone
- Distal tibia – Alternative site
- 1-2 cm proximal to medial malleolus
- Flat medial surface
- Distal femur – Alternative for infants
- Anterior surface, 1 cm above patella
- 10-15° cephalad angle
Needle Selection by Weight
| Weight | Age Estimate | Needle |
|---|---|---|
| 3-10 kg | Newborn to 12 months | 15mm Pink (may use manual) |
| 10-20 kg | 1-5 years | 15mm Pink |
| 20-39 kg | 5-12 years | 15mm Pink OR 25mm Blue |
| ≥40 kg | 12+ years | 25mm Blue |
Pediatric-Specific Technique Tips
- Support the extremity – Pediatric bones are more flexible
- Less force required – Cortex is thinner than adults
- Manual needles viable – Some prefer Jamshidi needles in infants
- Confirm placement carefully – Small marrow cavity, less marrow to aspirate
Fluid and Medication Dosing
- Lidocaine for conscious child: 0.5 mg/kg (max 40mg)
- Fluid bolus: 20 mL/kg; may repeat x3
- Epinephrine (arrest): 0.01 mg/kg (0.1 mL/kg of 1:10,000)
- All medications follow with 5 mL flush
Growth Plate Considerations
- The growth plate (physis) is located at the ends of long bones
- Proper IO sites are on the metaphysis, away from the physis
- Proximal tibia site naturally avoids growth plate
- No documented cases of growth disturbance from proper IO placement
Core Concepts
- IO access provides IV-equivalent drug and fluid delivery
- Onset and absorption times match intravenous administration
- Use when IV access fails after 2 attempts or 90 seconds
- First-line alternative access in cardiac arrest and critical shock
Site Selection Summary
- Adults: Proximal humerus (fastest flow) or proximal tibia
- Pediatrics: Proximal tibia (first choice) or distal tibia
- Avoid: Fractured bones, prior IO site, infected tissue
Procedure Essentials
- EZ-IO: Insert needle to bone surface, drill until loss of resistance
- Confirm: Needle stability, marrow aspirate, flush without resistance
- Lidocaine first for conscious patients (40mg adults, 0.5mg/kg peds)
- Use pressure bag for bolus fluids
- Remove within 24 hours
Critical Numbers
| Parameter | Value |
|---|---|
| Time to insertion | 10-30 seconds |
| Failed IV threshold | 2 attempts OR 90 seconds |
| Lidocaine dose (adult) | 40 mg slow push |
| Lidocaine dose (peds) | 0.5 mg/kg (max 40mg) |
| Humerus flow rate | ~5 L/hr under pressure |
| Tibia flow rate | ~1-2 L/hr under pressure |
| Maximum duration | 24 hours |
| Complication rate | <1% |
Guidelines
- American Heart Association. Advanced Cardiovascular Life Support (ACLS) Provider Manual. 2020.
- American Heart Association. Pediatric Advanced Life Support (PALS) Provider Manual. 2020.
- Teleflex. Arrow EZ-IO Intraosseous Vascular Access System. Instructions for Use. 2023.
Key Studies & Reviews
- Petitpas F, et al. "Use of intra-osseous access in adults: a systematic review." Crit Care. 2016;20:102.
- Pasley J, et al. "Intraosseous infusion rates under high pressure: A comparison of the FAST1, EZ-IO, and BIG." Prehosp Emerg Care. 2015;19(1):117-122.

