Endotracheal Intubation
Comprehensive endotracheal intubation guide for paramedics and nurses - equipment, technique, troubleshooting, and safety protocols.
Comprehensive endotracheal intubation guide for paramedics and nurses - equipment, technique, troubleshooting, and safety protocols.
Endotracheal intubation (ETI) is the placement of a flexible plastic tube (endotracheal tube or ETT) into the trachea through the mouth or nose to establish and maintain a patent airway. This advanced airway procedure is one of the most critical interventions in emergency medicine, critical care, and anesthesia.
Endotracheal intubation serves multiple vital functions:
Endotracheal intubation becomes necessary when less invasive airway management techniques are insufficient or contraindicated. Common scenarios include:
Failure to maintain or protect the airway:
Respiratory failure:
Trauma indications:
Medical emergencies:
Anticipated clinical course with high risk:
There are few absolute contraindications to intubation when it's truly indicated, but be cautious with:
Systematic airway assessment helps identify potential difficulties before the first laryngoscopy attempt. Use both structured scoring systems and clinical gestalt to predict structural difficulty ("Can I get the tube in?") and physiologic difficulty ("Can they tolerate the attempt?").
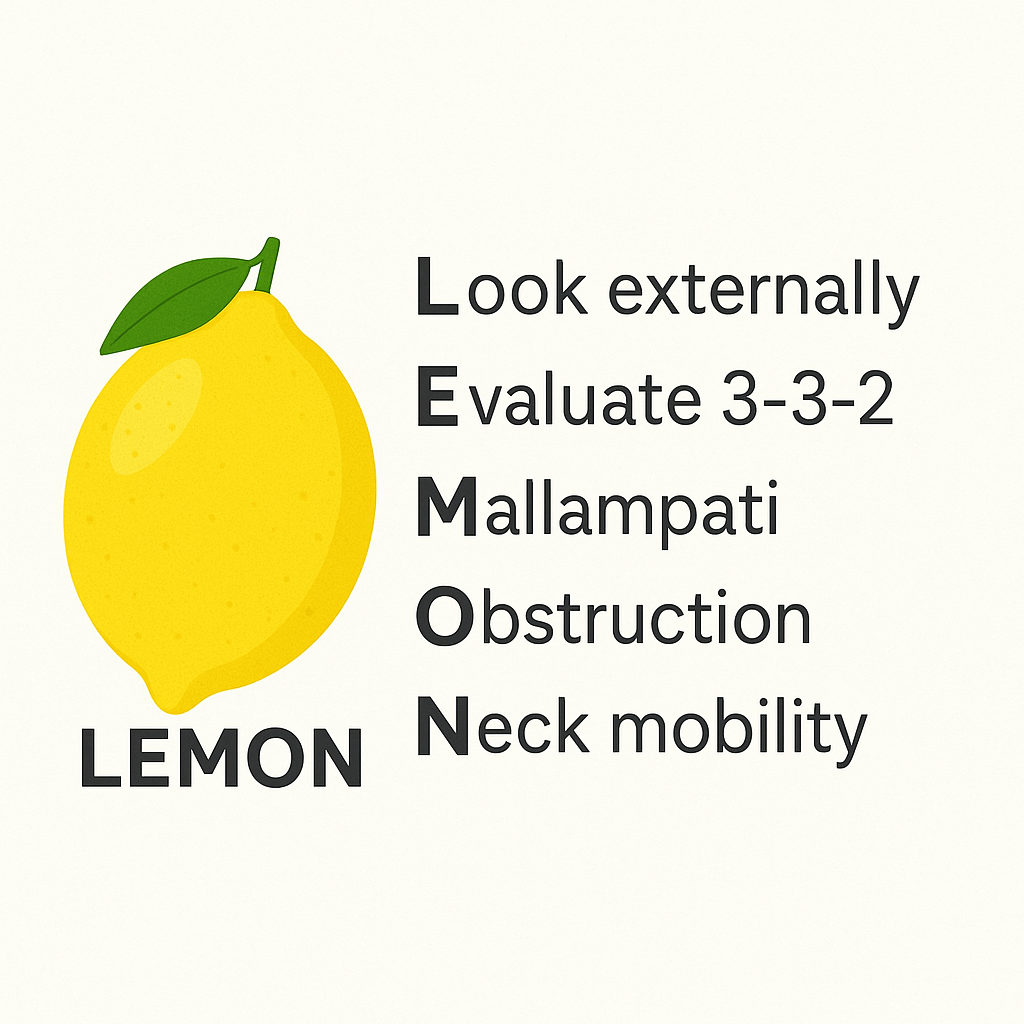
| Component | What to Assess | Concerning Findings |
|---|---|---|
| Look Externally | Facial appearance, anatomy | Facial trauma, large tongue, beard, missing teeth, obesity, limited mouth opening, prominent incisors |
| Evaluate 3-3-2 | Anatomic measurements | < 3 fingerbreadths mouth opening < 3 FB mentum to hyoid < 2 FB hyoid to thyroid notch |
| Mallampati | Oropharyngeal view (when possible) | Class III-IV (only soft palate visible, or soft palate not visible) |
| Obstruction | Airway patency | Tumor, hematoma, abscess, foreign body, angioedema, epiglottitis |
| Neck Mobility | Cervical spine movement | C-collar, ankylosing spondylitis, spinal fusion, pain/guarding, rheumatoid arthritis |
HEAVEN complements LEMON by identifying factors that increase procedural risk:
Assess the patient's physiologic reserve and ability to tolerate apnea during intubation:
Recognize these patients as extremely high-risk for peri-intubation complications:
Consider awake intubation, delayed sequence intubation (DSI), or other modified approaches for these patients.



| Blade Type | Technique | Sizes | Best Used For |
|---|---|---|---|
| Macintosh (Curved) | Sits in vallecula, indirectly lifts epiglottis by lifting hyoepiglottic ligament | 3 (standard adult), 4 (large adult) | Most adult intubations; larger mouth opening |
| Miller (Straight) | Directly lifts the epiglottis by placing blade tip posterior to it | 2 (small adult), 3 (standard adult) | Anterior larynx, pediatrics, floppy epiglottis |

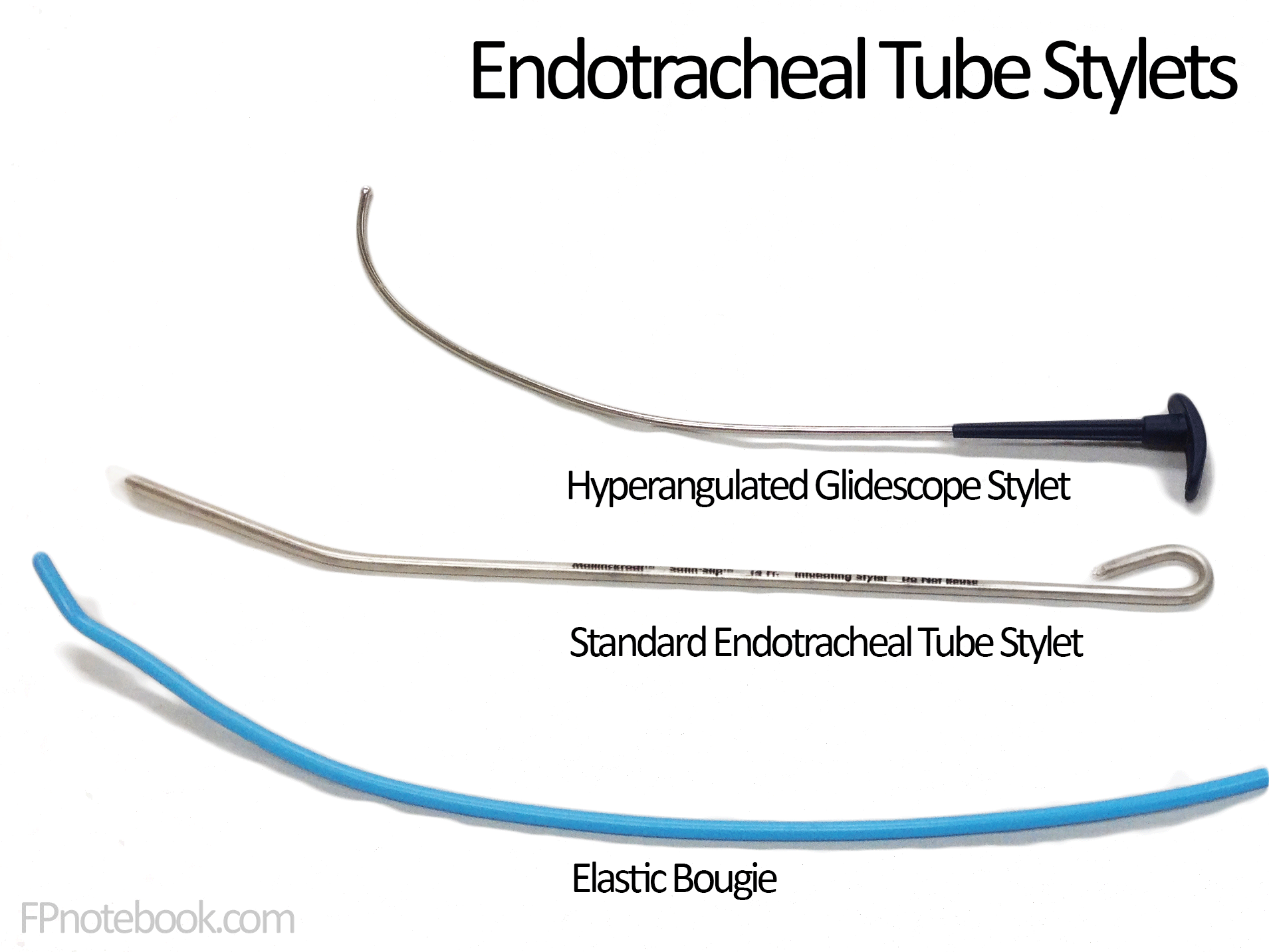
Stylet:
Bougie (Gum Elastic Bougie / Eschmann Introducer):
Suction:
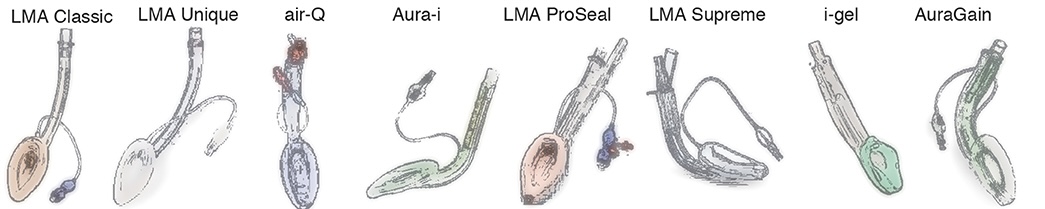
Supraglottic Airways (SGAs):

Before EVERY intubation, verify:
Before induction, conduct a brief team huddle:
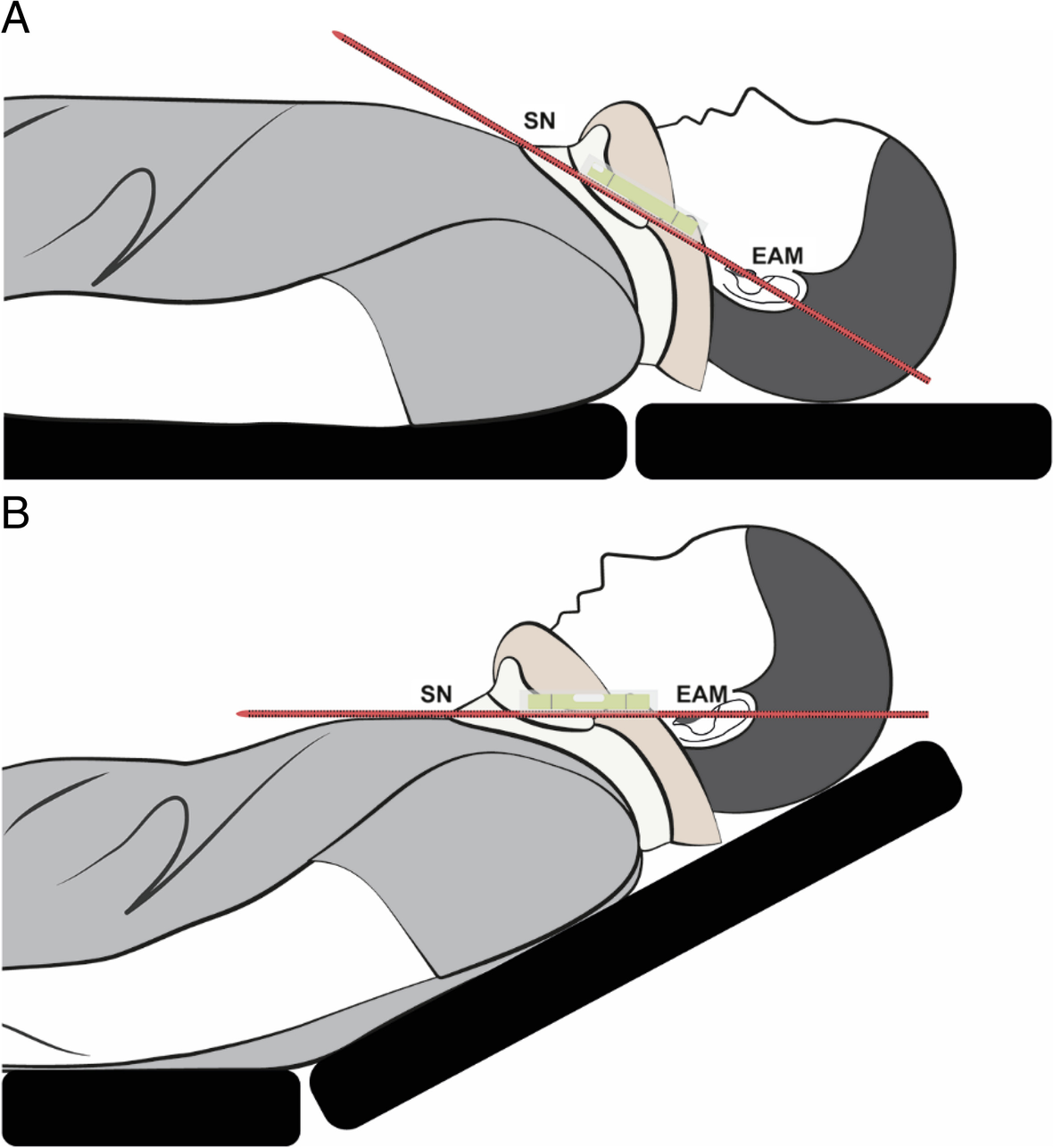
Ramped / Ear-to-Sternal-Notch Position:
Avoid flat supine positioning when possible:
Goal: Achieve SpO₂ ≥ 94% and maximize nitrogen washout to extend safe apnea time
The "sick, shocked, and pregnant" patient triad: These patients have dramatically reduced safe apnea times (often 1-2 minutes vs. 8+ minutes in healthy patients) due to:
Maximize preoxygenation time, consider delayed sequence intubation (DSI), and prepare for rapid desaturation.
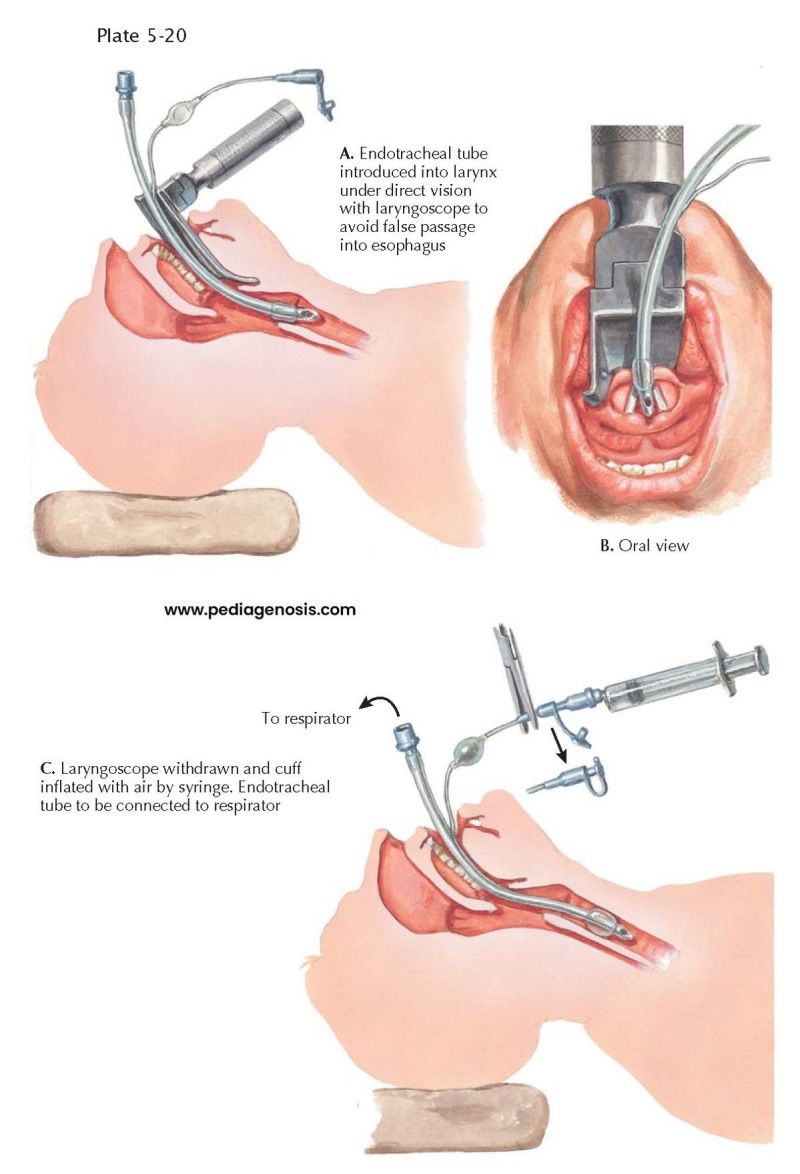
General Principles: Pre-brief that if SpO₂ drops below ~90% or attempt time approaches 20-30 seconds, the attempt will be aborted, BVM ventilation resumed, and the plan reassessed. RSI medications are chosen per your local protocol; this section focuses on the mechanical aspects of intubation.
Macintosh (Curved) Blade Technique:
Miller (Straight) Blade Technique:
Optimize the View:
If you have a good view (Cormack-Lehane Grade 1-2a):
If only partial view (Grade 2b-3: see arytenoids or epiglottis tip):
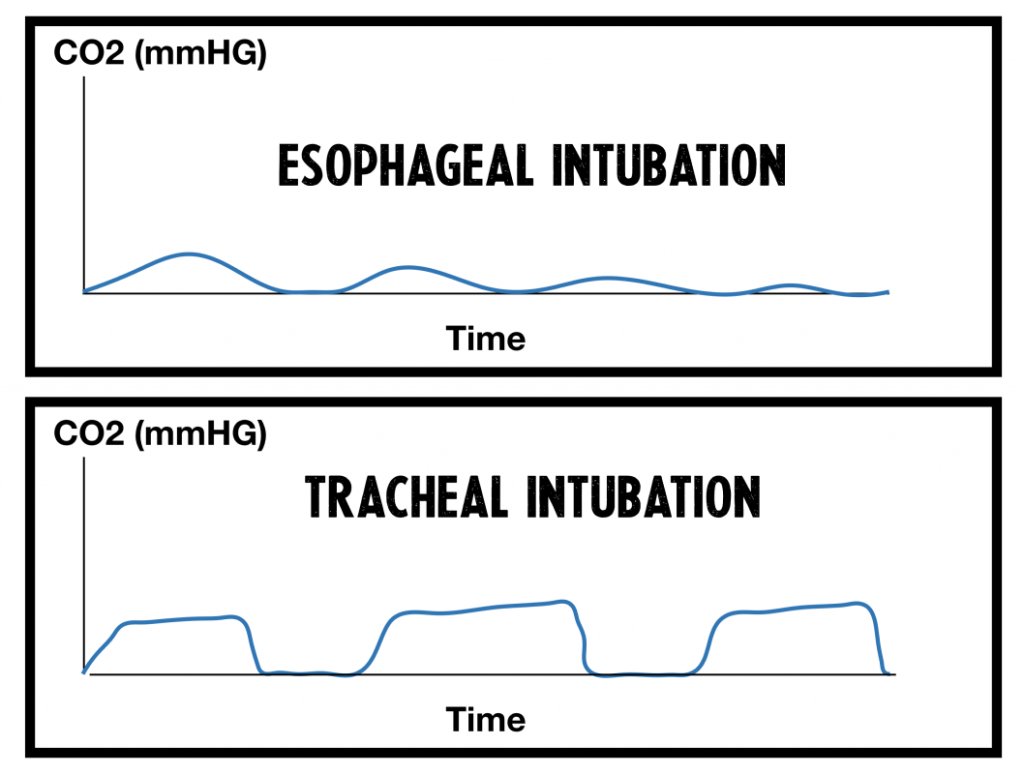
Primary confirmation - MUST HAVE:
Secondary confirmation:
Document:
The right mainstem bronchus is more vertical than the left, making it easy to advance the tube too far. Signs of right mainstem intubation:
Fix: Deflate cuff, withdraw tube 1-2 cm while auscultating, reinflate cuff, reassess. Typical adult depth is 21-23 cm at teeth (3x ETT internal diameter is a useful rule).
Capnography is the primary tool for confirming endotracheal tube placement and monitoring ongoing ventilation status. Waveform analysis provides real-time feedback on tube position, ventilation adequacy, circuit problems, and patient physiology.
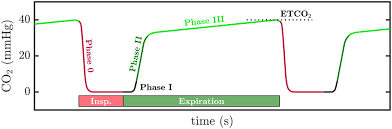
Four phases of normal waveform:
Normal EtCO₂ values: 35-45 mmHg in a perfusing patient (slightly lower than arterial PaCO₂ due to alveolar dead space)
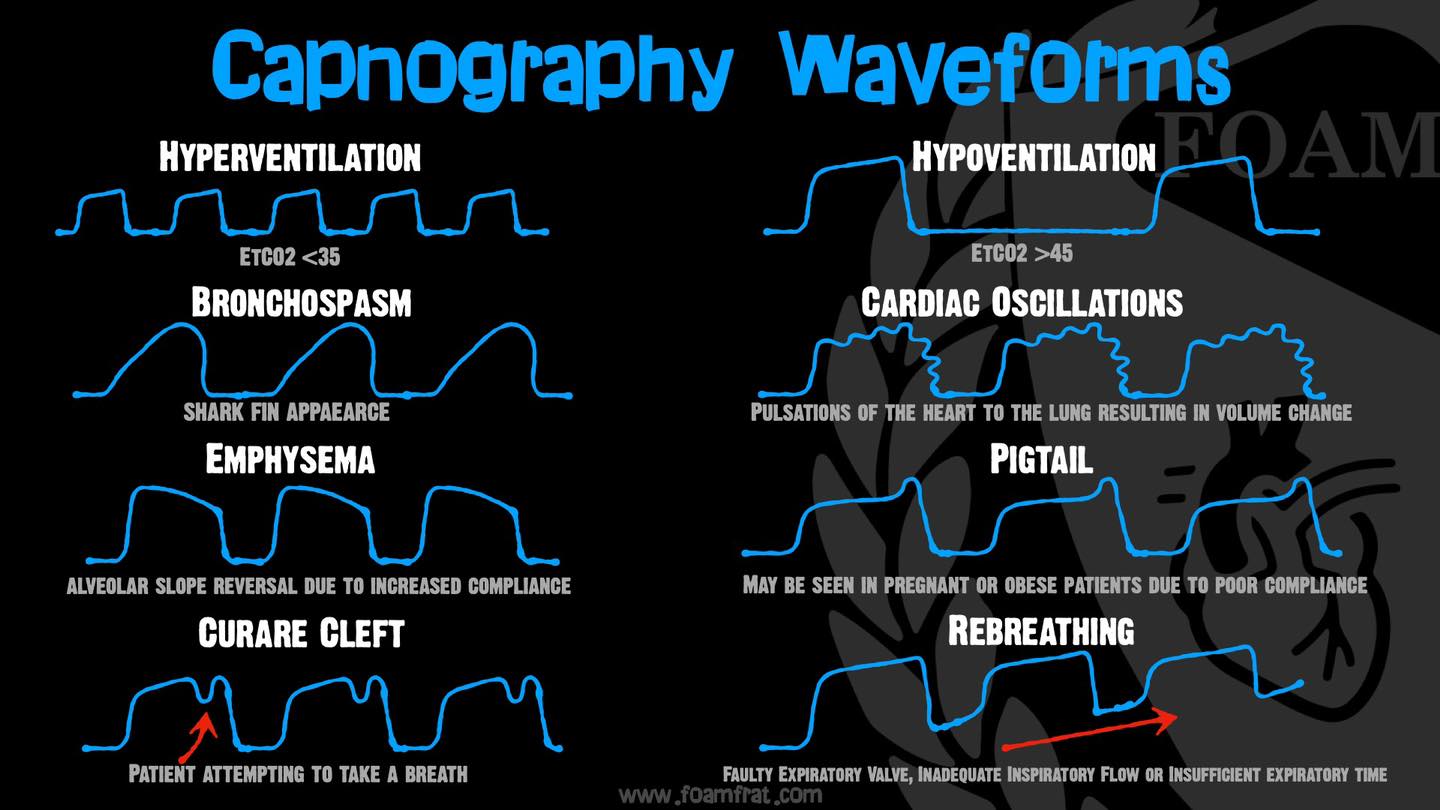
Think DOPE/DOPES:
| Problem | Signs | Action |
|---|---|---|
| Dislodged tube | Sudden loss of waveform, absent breath sounds, gurgling over stomach | Remove tube, reoxygenate with BVM, re-intubate |
| Obstruction | High peak pressures, no chest rise, kinked tube, biting, mucus plug | Suction, pass catheter through tube, adjust bite block, bronchodilators if bronchospasm |
| Pneumothorax | Unilateral absent breath sounds, hypotension, high pressures, neck vein distension | Needle decompression or chest tube, reassess ventilation |
| Equipment failure | Check capnograph, circuit disconnection, ventilator malfunction | Switch to BVM, replace circuit, check all connections |
| Stacked breaths / hypoventilation | Auto-PEEP, inadequate expiratory time | Decrease respiratory rate, increase expiratory time, check for air trapping |
EtCO₂ during CPR provides real-time feedback on resuscitation quality:
For average adult (ARDS or general critical care patient):
Continuous monitoring:
Periodic assessments:
Common and dangerous complication occurring in up to 25% of emergency intubations. Causes include:
Prevention/Management: Optimize volume status before intubation, use push-dose pressors, minimize PEEP/respiratory rate if hemodynamic instability develops.
Re-optimize positioning:
Change equipment:
Improve the field:
Use a bougie early:
Adjust the tube/stylet:
Optimize visualization:
Consider bougie-assisted:
Prioritize oxygenation over intubation:
Place supraglottic airway early (Plan B):
Alternative intubation strategies:
Declare CICO emergency out loud:
Criteria for declaring CICO:
Proceed immediately to surgical airway (Plan C):
Multiple failed attempts with worsening hypoxemia, hypotension, and acidosis create a vicious cycle. Each attempt becomes more difficult as the patient deteriorates. Prevent this by:
"Failing to plan is planning to fail" is never more true than in emergency airway management.