Hemodialysis (HD)
Comprehensive hemodialysis guide for paramedics and nurses - principles, vascular access, complications, and patient care.
Comprehensive hemodialysis guide for paramedics and nurses - principles, vascular access, complications, and patient care.
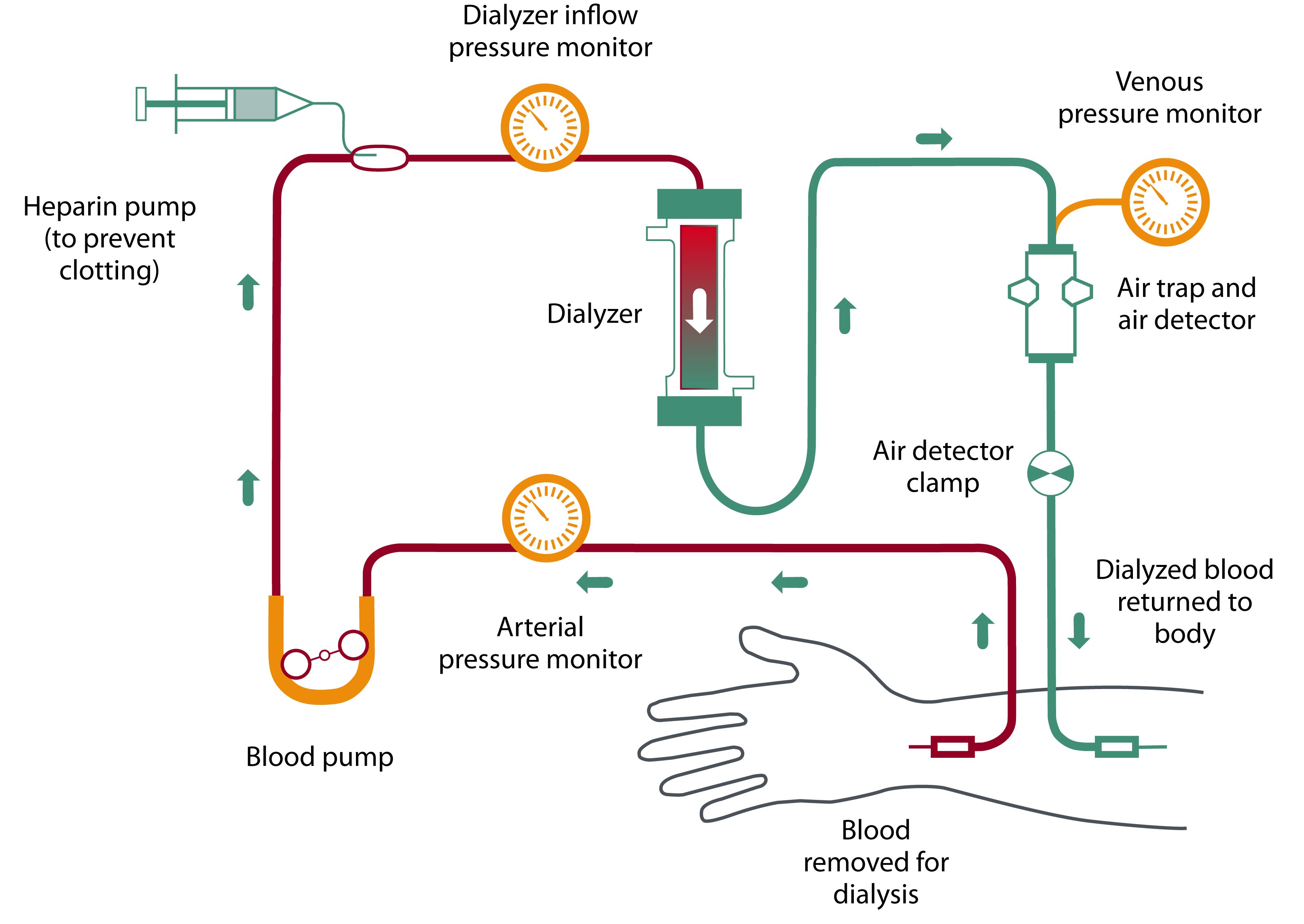
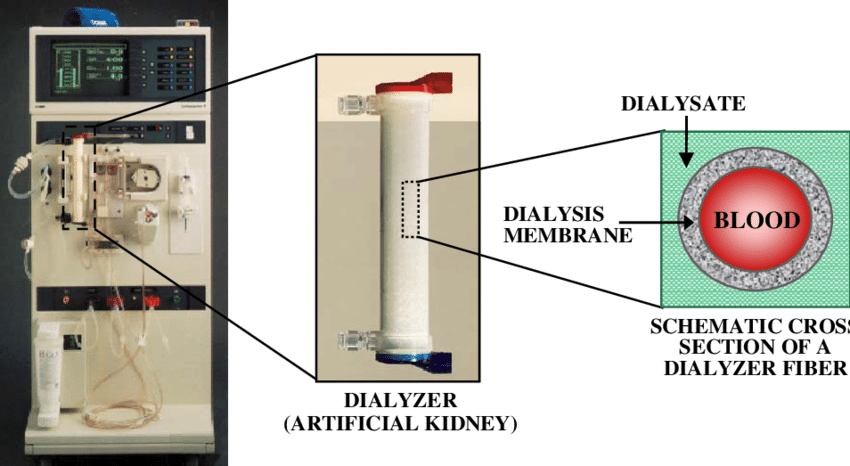
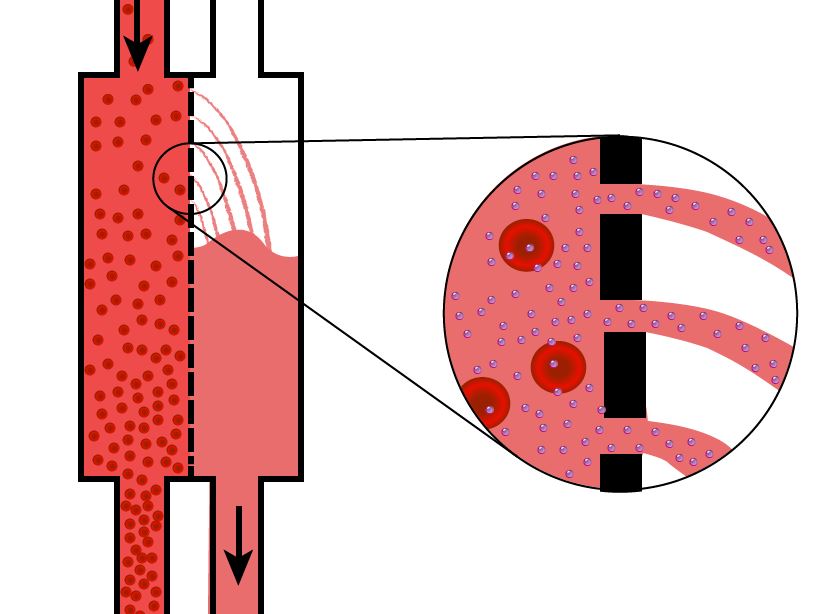
Hemodialysis (HD) is a form of renal replacement therapy (RRT) that uses an extracorporeal circuit and a semipermeable membrane (dialyzer) to remove toxins, correct electrolytes and acid-base disturbances, and remove excess fluid from the blood.
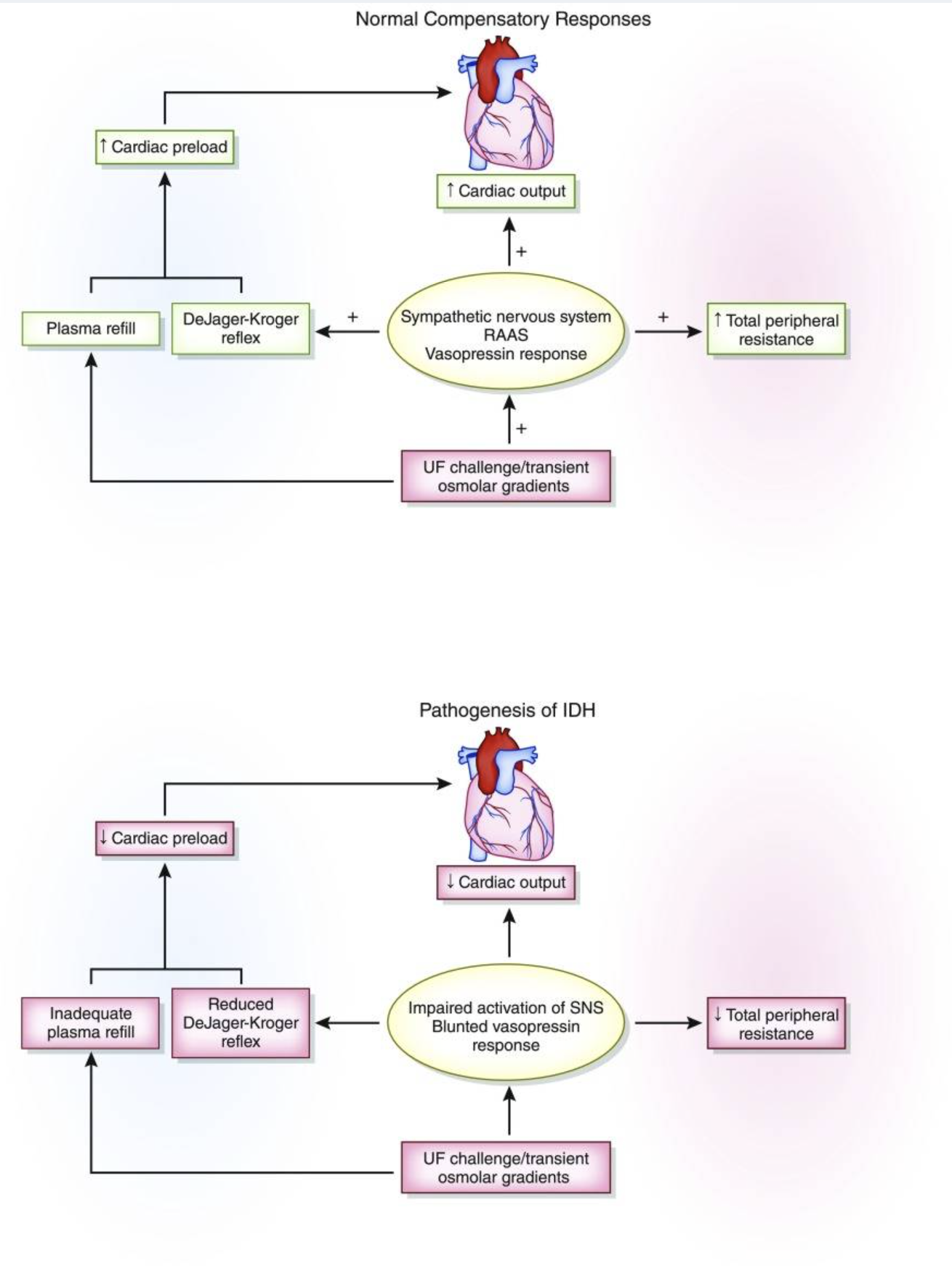
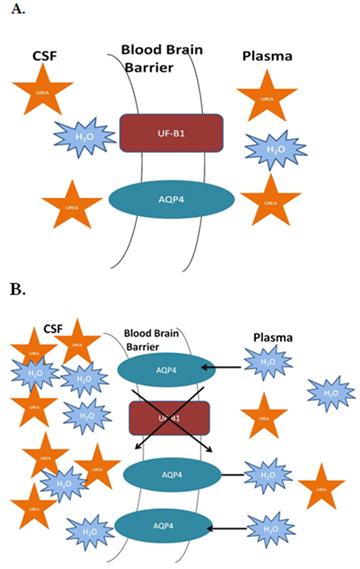
In HD, blood is pumped from the patient through a dialyzer where solute exchange occurs between blood and dialysate (a carefully composed fluid) via diffusion and convection. The "cleaned" blood is then returned to the patient.
HD is used both chronically (end-stage kidney disease, ESKD) and acutely (acute kidney injury, AKI) in hospital settings. In ED/ICU/transport environments, you most often encounter patients who are either:
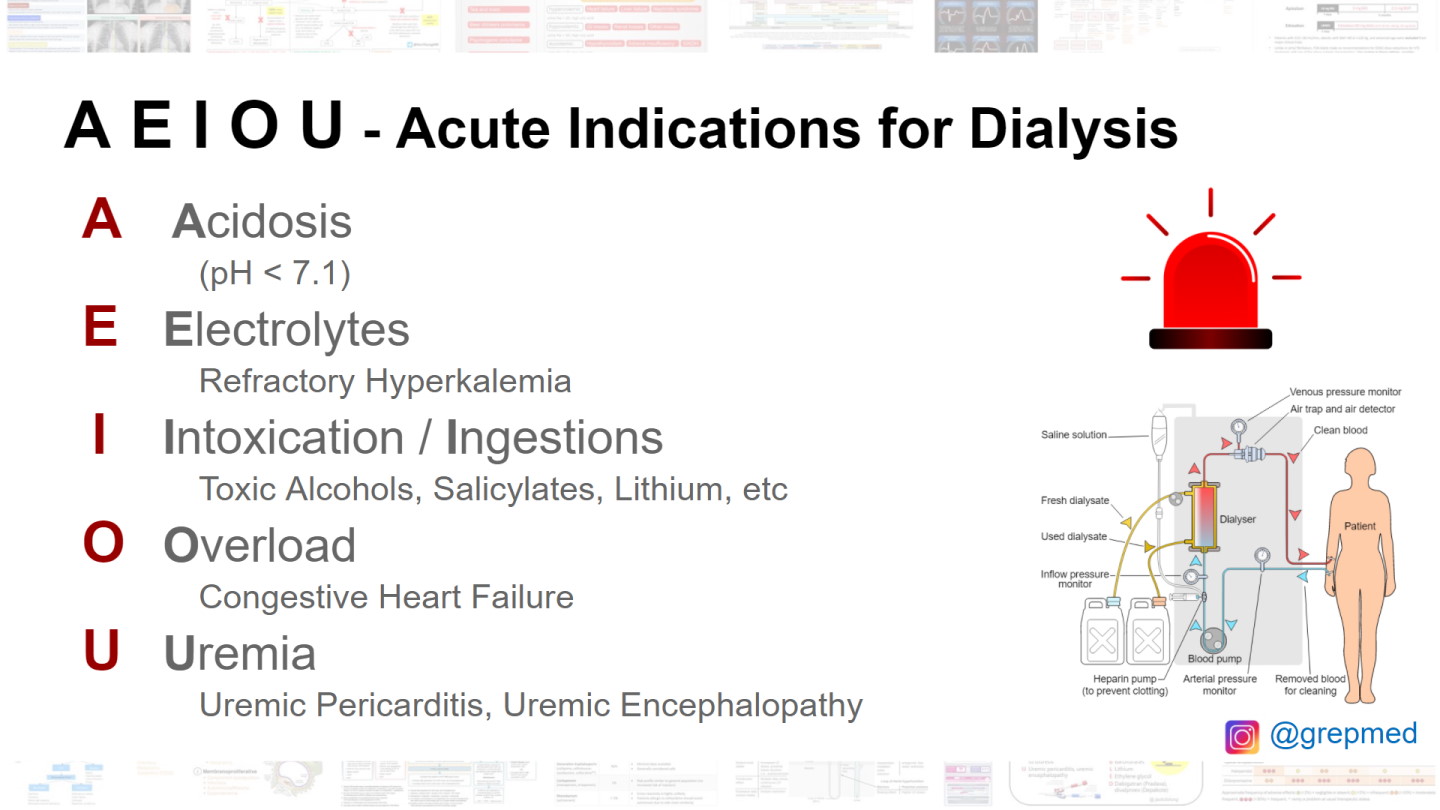
Classic emergent indications are often remembered with the mnemonic "AEIOU":
A nephrologist writes the detailed HD prescription, but bedside providers should recognize the major components:
E.g., chronic HD 3 times per week, 3–5 hours per session; more frequent/shorter or extended sessions in ICU depending on tolerability.
Often 300–500 mL/min on chronic HD; may be lower in ICU or with limited access.
Commonly ~500–800 mL/min; higher flows increase clearance.
Often systemic unfractionated heparin bolus plus smaller maintenance doses; alternatives include regional citrate or heparin-free dialysis in patients with active bleeding or high risk.