Medical Disclaimer
- For Educational Purposes Only: This content is intended for educational reference and should not be used for clinical decision-making.
- Not a Substitute for Professional Judgment: Always consult your local protocols, institutional guidelines, and supervising physicians.
- Verify Before Acting: Users are responsible for verifying information through authoritative sources before any clinical application.
AI Assistance Notice
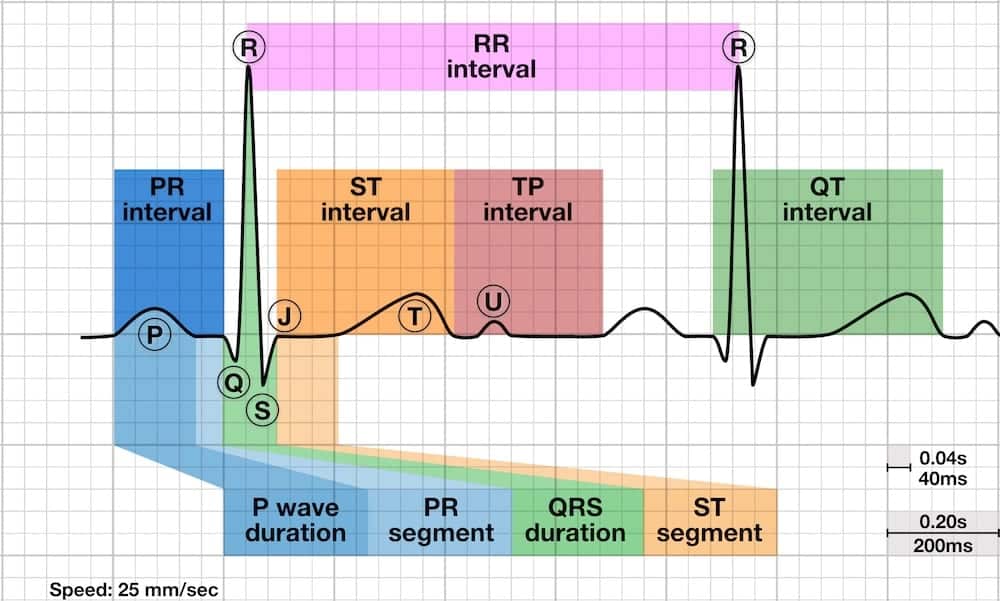
The QT interval represents the total time for ventricular depolarization and repolarization - essentially the duration of ventricular systole from the start of ventricular contraction to complete relaxation. It begins at the onset of the QRS complex and ends when the T wave returns to the isoelectric baseline.
Understanding the QT interval is critical because:
- Prolonged QT: Associated with increased risk of life-threatening ventricular arrhythmias, particularly Torsades de Pointes (polymorphic VT)
- Shortened QT: Less common but associated with sudden cardiac death from atrial and ventricular fibrillation
- Heart rate dependent: QT naturally shortens with faster heart rates and lengthens with slower rates - must be corrected (QTc)
- Reversible causes: Electrolyte abnormalities and medications are common culprits that can be identified and treated
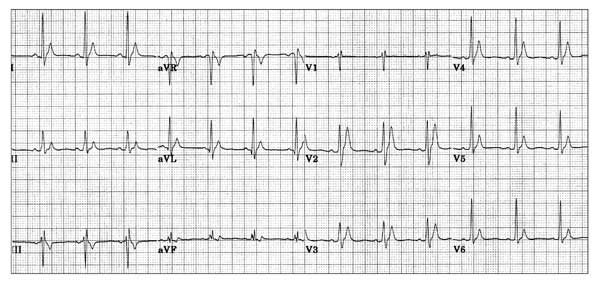
Measurement Technique
Accurate QT measurement requires careful technique:
- Choose the right lead: Measure in lead II or V5-V6 (these typically have the most prominent T waves). Use the lead with the longest QT interval
- Measure multiple beats: Assess several consecutive complexes and use the maximum (longest) interval
- Define the start: Beginning of the QRS complex (onset of Q wave, or R wave if no Q is present)
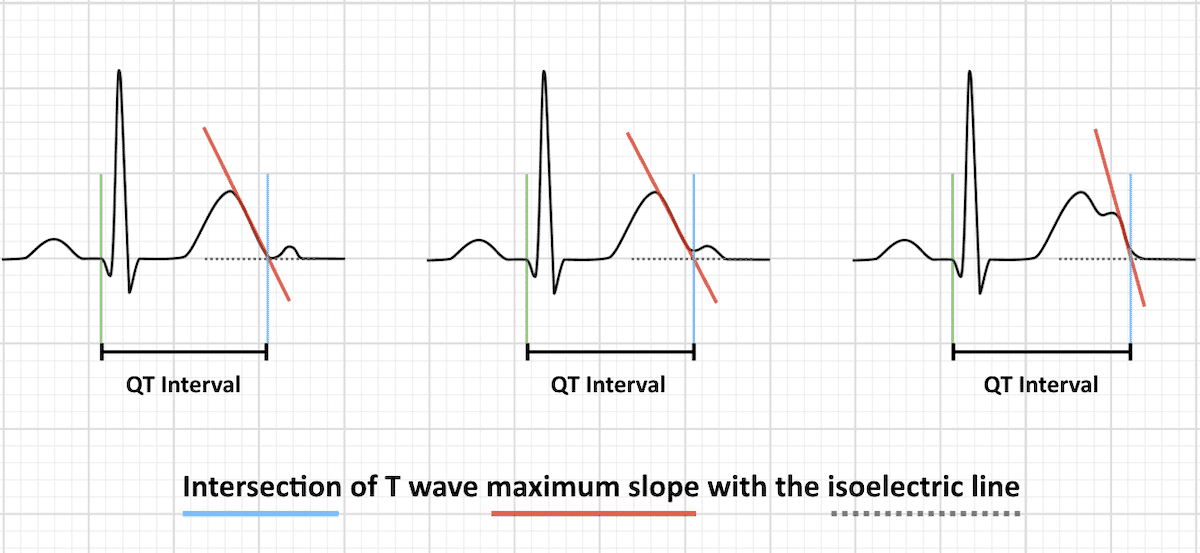
- Define the end: Use the maximum slope intercept method - where the steepest downslope of the T wave intersects the isoelectric baseline
- Avoid the PR segment: Do not include the PR interval in your measurement
Dealing with U Waves
- Large U waves (>1mm) fused to T wave: Include in the QT measurement
- Small or separate U waves: Exclude from the measurement - measure only to the end of the T wave
- When uncertain: Use the nadir (lowest point) between the T and U waves as the end of the T wave
Why Correction is Necessary
The QT interval is inversely proportional to heart rate:
- Faster heart rates → shorter QT intervals
- Slower heart rates → longer QT intervals
- To assess for abnormal prolongation or shortening, we must correct for heart rate
- QTc estimates what the QT interval would be at a standardized heart rate of 60 bpm
Correction Formulas
Multiple formulas exist to calculate QTc. The RR interval is measured in seconds (RR = 60 / heart rate).
| Formula | Equation | Best Use Case | Limitations |
|---|---|---|---|
| Bazett | QTc = QT / √RR | HR 60-100 bpm | Over-corrects at HR >100; under-corrects at HR <60 |
| Fridericia | QTc = QT / ∛RR | HR <60 or >100 bpm | More accurate than Bazett at extreme heart rates |
| Framingham | QTc = QT + 0.154 (1 – RR) | Linear correction | Less commonly used clinically |
| Hodges | QTc = QT + 1.75 (HR – 60) | Linear correction | Uses heart rate directly (not RR interval) |
- Bazett formula: Most commonly used due to simplicity. Adequate for HR 60-100 bpm. Built into most ECG machines.
- Fridericia formula: More accurate outside the 60-100 bpm range. Use when heart rate is very slow or very fast.
- If HR = 60 bpm: No correction needed! The absolute QT = QTc.
Reference Ranges
| Category | QTc Range | Clinical Significance |
|---|---|---|
| Normal (Men) | <440 ms | No increased arrhythmia risk from QT duration |
| Normal (Women) | <460 ms | Women have slightly longer baseline QTc than men |
| Borderline Prolonged | 440-500 ms | Mild increased risk; evaluate for reversible causes |
| Prolonged (High Risk) | >500 ms | Significantly increased risk of Torsades de Pointes |
| Short QTc | <350 ms | Increased risk of AF, VF, and sudden cardiac death |
Rule of Thumb
Risk Stratification for Torsades de Pointes
- QTc <440 ms: Low risk (baseline population risk)
- QTc 440-500 ms: Mild increased risk - monitor closely, address reversible causes
- QTc 500-550 ms: Moderate-high risk - consider telemetry, correct electrolytes, review medications
- QTc >550 ms: Very high risk - continuous monitoring, aggressive electrolyte repletion, discontinue QT-prolonging drugs, consider cardiology consult
QT prolongation can result from a wide variety of causes. The mnemonic "ELECTROLYTES" captures many reversible causes:
- Electrolyte abnormalities (↓K+, ↓Mg2+, ↓Ca2+)
- Long QT syndrome (congenital)
- Elevated intracranial pressure
- Cardiac (ischemia, myocarditis, cardiomyopathy)
- Temperature (hypothermia)
- ROSC (return of spontaneous circulation) post-arrest
- Other drugs (see below)
- Liver failure
- Yield to medications (antiarrhythmics, psychotropics, antibiotics)
- Toxins (organophosphates)
- Endocrine (hypothyroid)
- Starvation/anorexia
Electrolyte Abnormalities
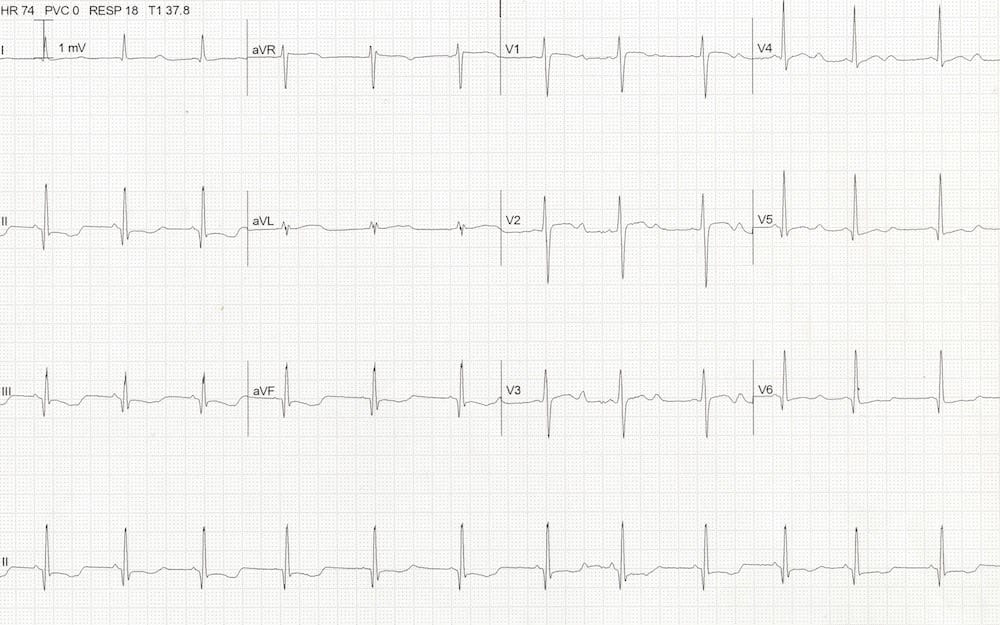
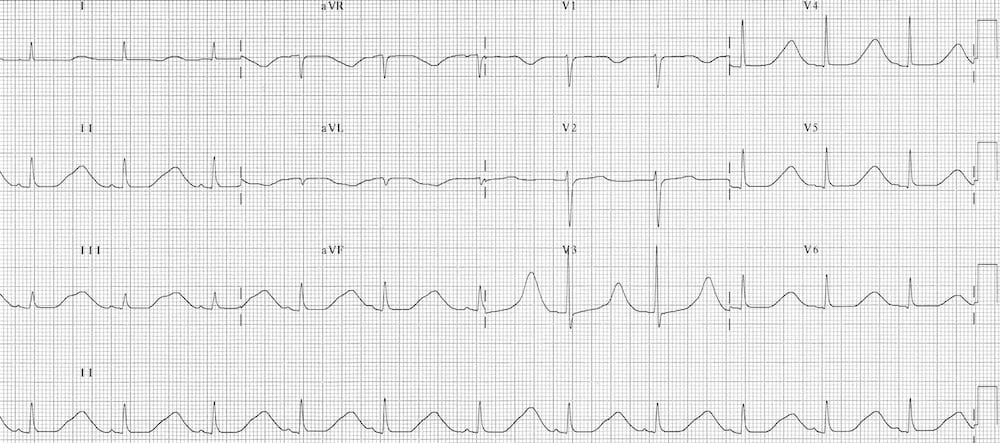
Hypokalemia
The most common electrolyte cause of QT prolongation.
- Mechanism: Reduced K+ slows repolarization, prolonging phase 3 of the action potential
- ECG features: Apparent QTc prolongation (often due to T-U fusion), prominent U waves in precordial leads, ST depression, T wave flattening
- Clinical significance: Risk increases dramatically when K+ <3.0 mEq/L
Hypomagnesemia
- Mechanism: Mg2+ deficiency impairs K+ channel function and prolongs repolarization
- Often coexists: With hypokalemia (Mg2+ is required for K+ repletion)
- Treatment: Correct Mg2+ before or alongside K+ replacement
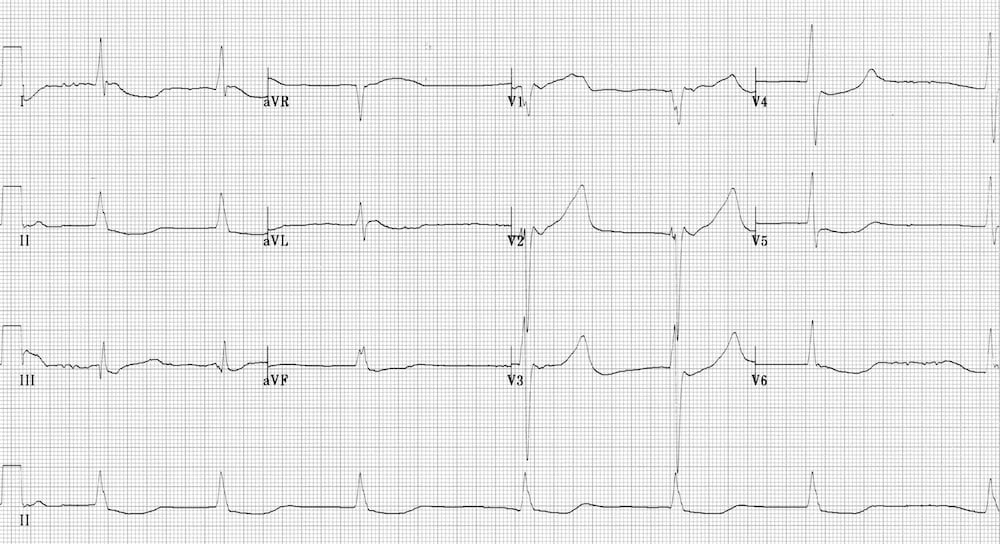
Hypocalcemia
- Mechanism: Low Ca2+ prolongs the plateau phase (phase 2) of the action potential
- Unique feature: Prolongation is primarily in the ST segment, leaving the T wave relatively unchanged
- Look for: Long, flat ST segment with normal or prolonged QT
Hypothermia
- Mechanism: Cold slows all cardiac electrical activity
- ECG features: Marked QTc prolongation, bradycardia, Osborn waves (J waves), shivering artifact, atrial arrhythmias
- Severity: Prolongation worsens with decreasing temperature; QTc >600ms common in severe hypothermia
Myocardial Ischemia & Infarction
- Mechanism: Ischemic myocardium has delayed and heterogeneous repolarization
- Typical range: Modest QTc prolongation, usually 450-500ms
- Clinical utility: Can help distinguish hyperacute STEMI from benign early repolarization (BER). Hyperacute MI typically has prolonged QTc; BER usually has normal QTc
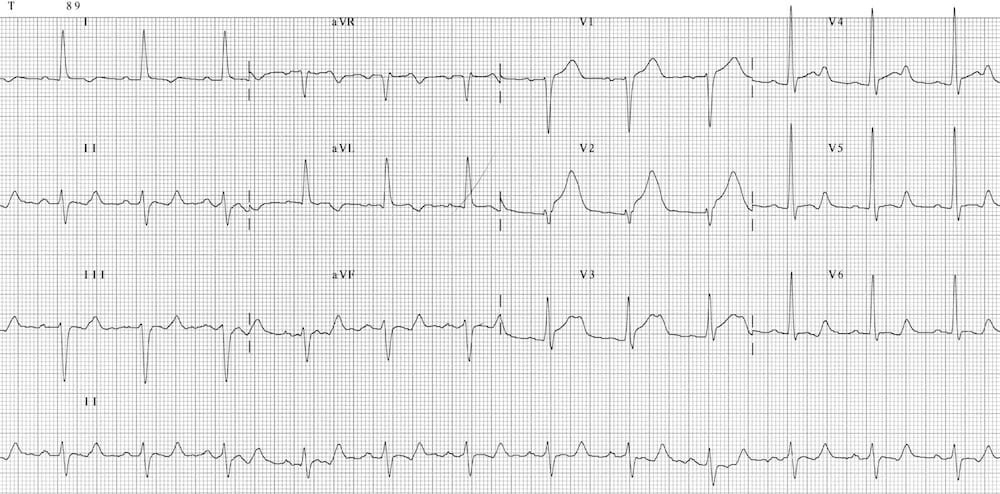
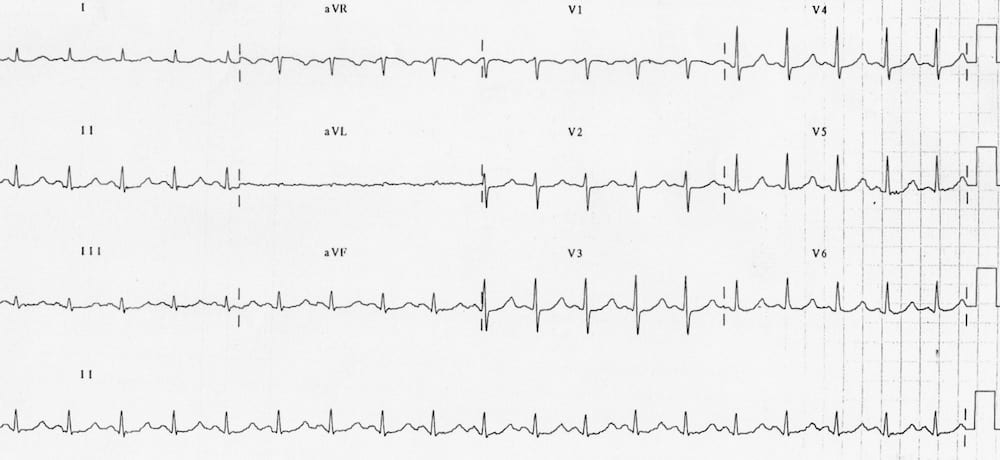
Raised Intracranial Pressure
- Mechanism: Autonomic surge from sudden ICP elevation causes "cerebral T waves"
- Classic association: Subarachnoid hemorrhage
- ECG features: Widespread, deep T wave inversions with markedly prolonged QTc (often >600ms)
- Key point: These changes do NOT represent primary cardiac disease but neurogenic effect on the heart
Congenital Long QT Syndrome
- Mechanism: Inherited channelopathies affecting cardiac ion channels (K+, Na+, Ca2+)
- Multiple subtypes: LQTS 1-3 are most common (each with different triggers and T wave morphology)
- Clinical significance: High risk of syncope, Torsades de Pointes, and sudden cardiac death
- Triggers vary by type: Exercise (LQTS1), auditory stimuli (LQTS2), rest/sleep (LQTS3)
- Treatment: Beta-blockers, lifestyle modifications, ICD in high-risk patients

Medications Causing QT Prolongation
Numerous medications prolong the QT interval. Common culprits include:
| Drug Class | Common Examples |
|---|---|
| Antiarrhythmics | Amiodarone, sotalol, dofetilide, ibutilide, quinidine, procainamide |
| Antipsychotics | Haloperidol, quetiapine, ziprasidone, chlorpromazine |
| Antidepressants | Citalopram, escitalopram, tricyclics (amitriptyline, nortriptyline) |
| Antibiotics | Fluoroquinolones (levofloxacin, moxifloxacin), macrolides (azithromycin, erythromycin) |
| Antifungals | Fluconazole, ketoconazole |
| Antiemetics | Ondansetron, droperidol |
| Opioids | Methadone (especially high doses) |
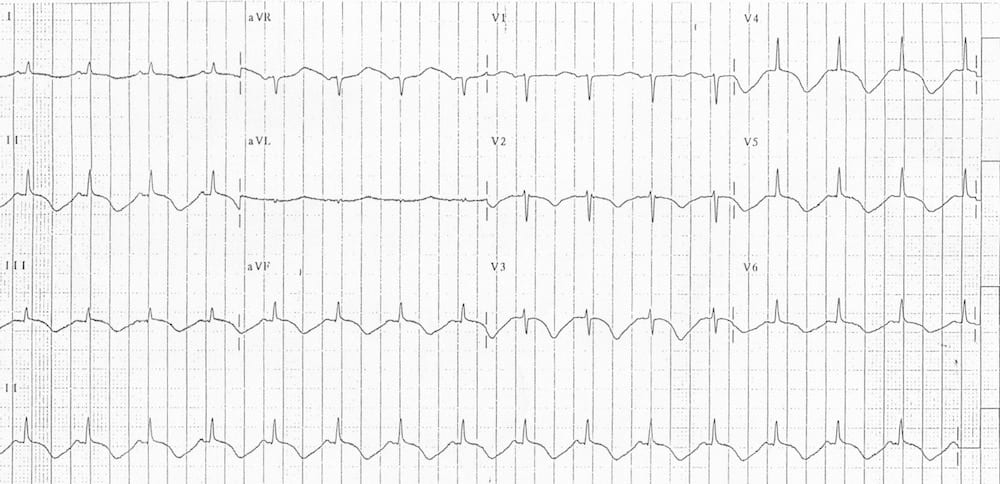
Short QT syndrome is less common than prolonged QT but is equally dangerous, associated with increased risk of atrial fibrillation, ventricular fibrillation, and sudden cardiac death.
Hypercalcemia
- Mechanism: Elevated Ca2+ shortens the plateau phase (phase 2) of the action potential
- ECG features: Shortened ST segment (most prominent), short QTc, may see Osborn waves
- Causes: Hyperparathyroidism, malignancy, vitamin D toxicity, immobilization

Congenital Short QT Syndrome (SQTS)
- Mechanism: Autosomal dominant inherited disorder of potassium channels (gain of function mutations)
- ECG features: Very short QTc (<300-350ms), tall peaked T waves, failure of QT to lengthen appropriately with slower heart rates
- Clinical significance: High risk of paroxysmal atrial and ventricular fibrillation, sudden cardiac death at young age
- Diagnostic clues: Family history of sudden death, lone AF in young adults, syncope
Digoxin Effect
- Mechanism: Inhibition of Na+/K+ ATPase shortens repolarization
- ECG features: Relative QT shortening, "reverse tick" ST depression (downward sloping ST in lateral leads), T wave flattening/inversion, increased arrhythmias
- Note: Digoxin effect (therapeutic) is different from digoxin toxicity (life-threatening arrhythmias)
The QT Nomogram
In the context of acute poisoning or drug overdose with QT-prolonging agents, the absolute QT interval (not QTc) better predicts Torsades de Pointes risk.
- Developed by Chan et al (2007): A clinically validated tool for risk stratification in drug-induced QT prolongation
- How to use: Plot the QT interval (ms) and heart rate (bpm) from the same ECG as a coordinate pair
- Interpretation: Points that fall above the line indicate the patient is at risk of Torsades de Pointes
- Clinical utility: More accurate than QTc alone in poisoning/overdose scenarios
Management of Drug-Induced QT Prolongation
- Discontinue offending agent(s): Stop all QT-prolonging medications if possible
- Correct electrolytes: Target K+ >4.0 mEq/L, Mg2+ >2.0 mg/dL
- Continuous monitoring: Telemetry or ICU monitoring for high-risk patients
- Avoid bradycardia: Slower heart rates worsen QT prolongation (consider pacing if symptomatic and bradycardic)
- If Torsades develops: Immediate defibrillation if unstable; IV magnesium 2g bolus; overdrive pacing or isoproterenol
- Definition: Time from Q wave start to T wave end - represents ventricular depolarization through repolarization
- Normal QTc: <440ms (men), <460ms (women)
- Prolonged QTc: >440ms (men) or >460ms (women) - risk of Torsades de Pointes increases dramatically >500ms
- Short QTc: <350ms - increased risk of atrial and ventricular fibrillation
- Rule of thumb: Normal QT should be less than half the preceding RR interval
- Correction needed: QT varies with heart rate - must use corrected QT (QTc) for accurate interpretation
- Key pearl: QTc >500ms = high risk for Torsades; always check electrolytes (K+, Mg2+, Ca2+) and medication list
- Farkas, Josh MD. (2015). Table of Contents - EMCrit Project. EMCrit Project. https://emcrit.org/ibcc/toc/
- Khan, M. G. (2007). Rapid ECG Interpretation. Humana.
- Sigg, D. C., Iaizzo, P. A., Xiao, Y.-F., Bin He, & Springerlink (Online Service). (2010). Cardiac Electrophysiology Methods and Models. Springer Us.
- Wang, K. (2012). Atlas of Electrocardiography. JP Medical Ltd.
- ECG Library • LITFL • ECG Library Basics. (2018). Life in the Fast Lane • LITFL • Medical Blog. https://litfl.com/ecg-library/

