Mechanical Circulatory Support
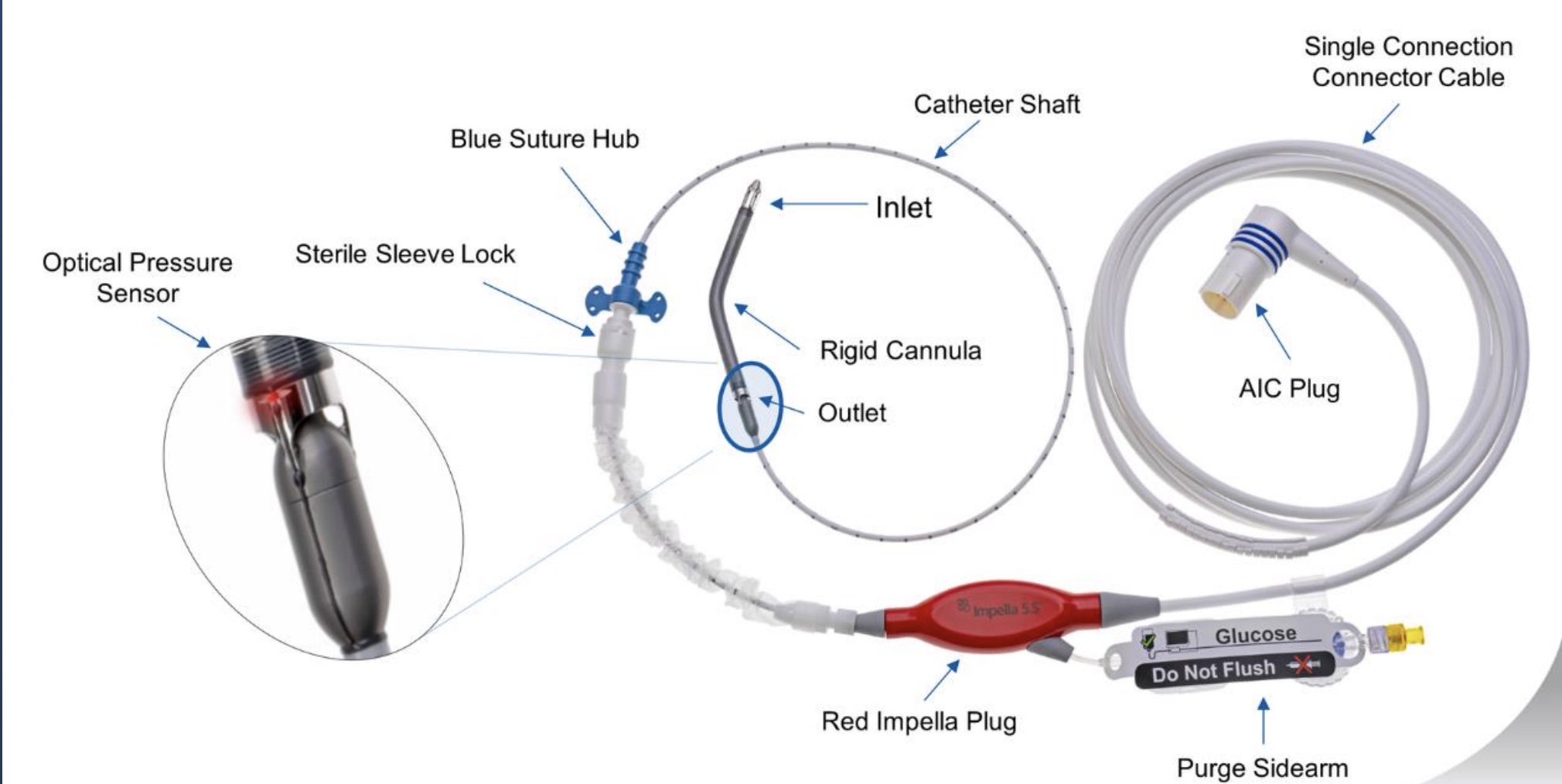
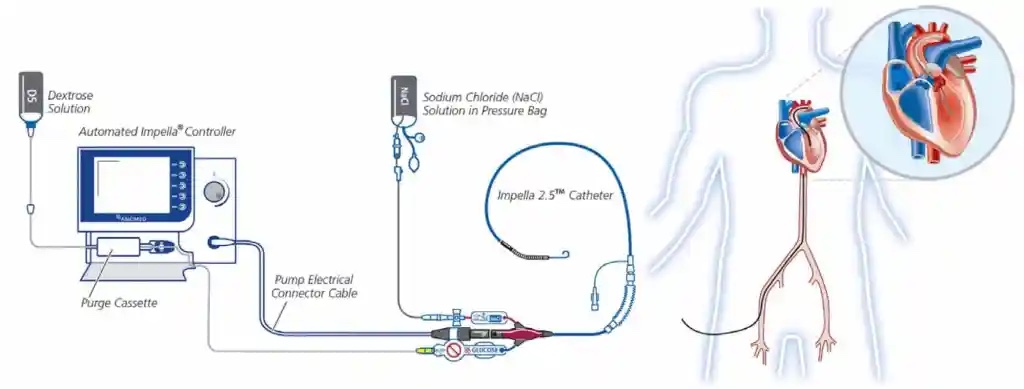
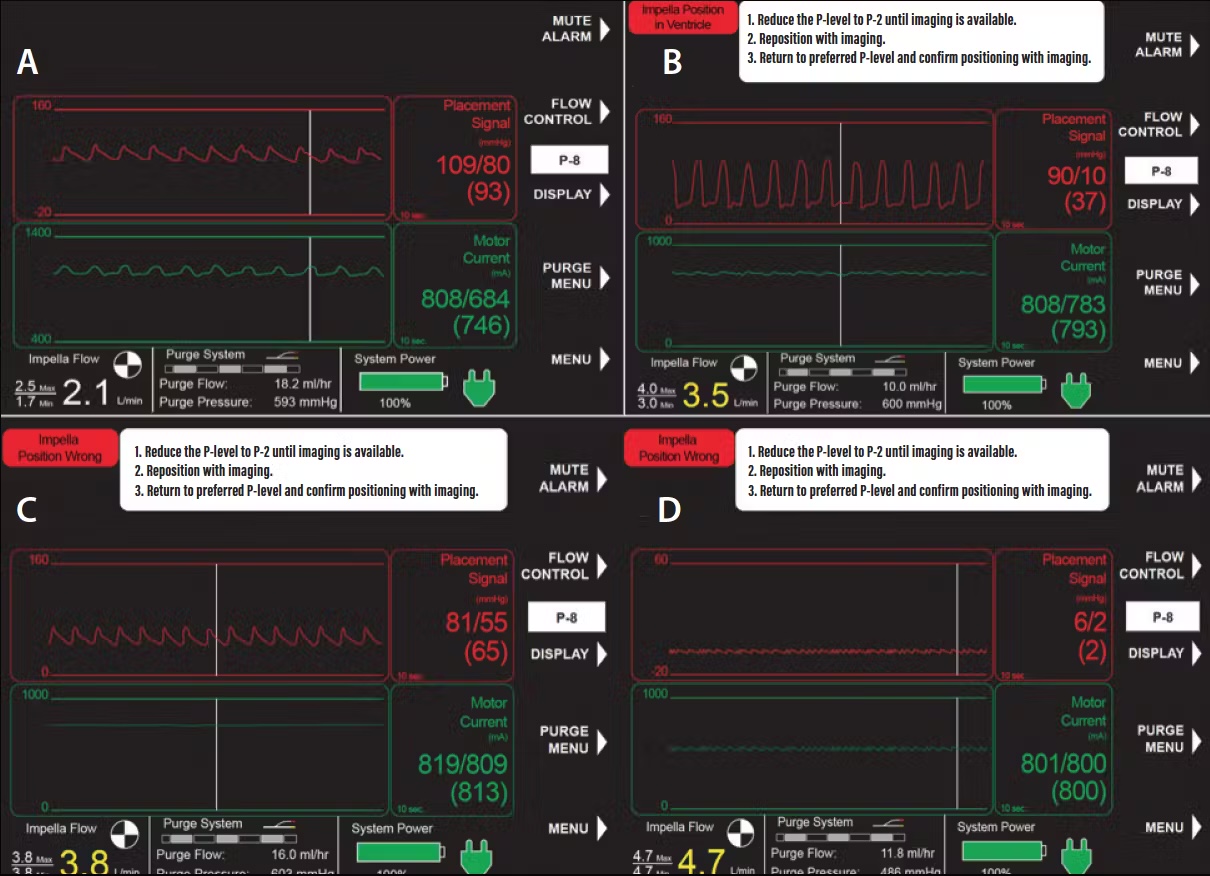
Impella Devices
Microaxial ventricular assist device for LV & RV support. Pulls blood from LV and ejects into ascending aorta for direct unloading and forward flow.
2.5-6.0
L/min Support
CP/5.0/5.5
Device Options
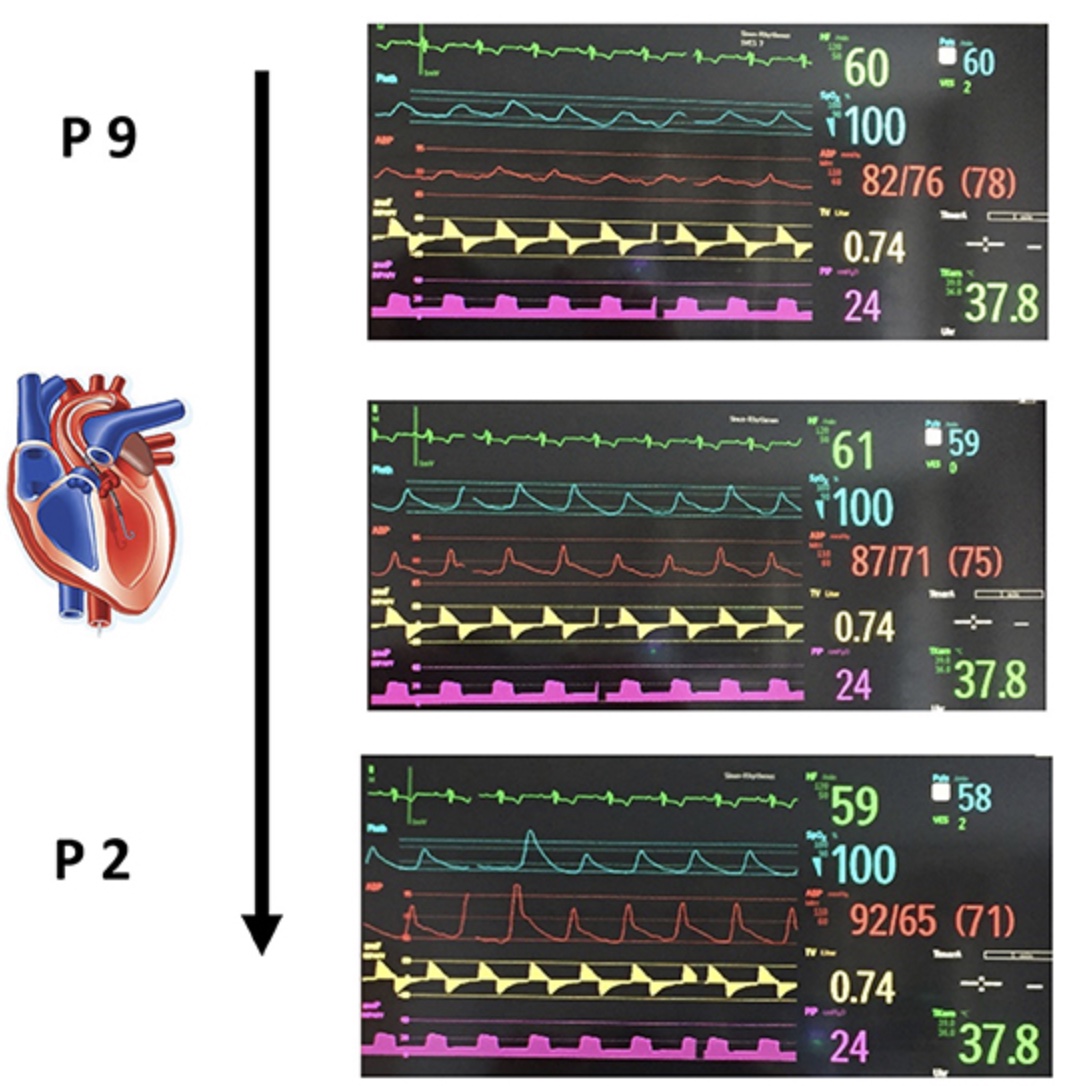
P2-P9
Power Levels