Cardiopulmonary Support & Monitoring
Extracorporeal Membrane Oxygenation (ECMO)
VV & VA Extracorporeal Life Support | ICU Reference for Critical Care Paramedics & Nurses
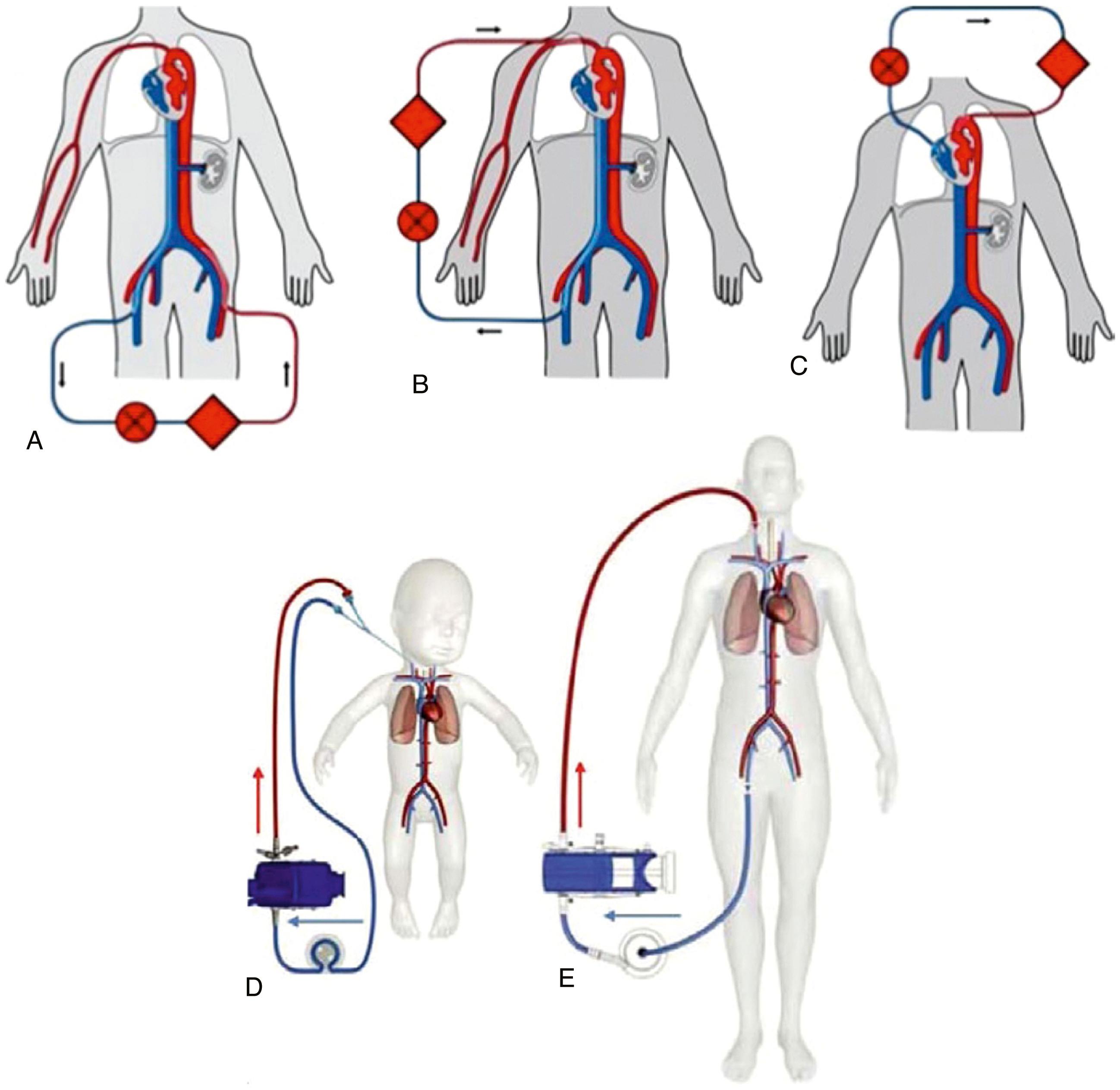
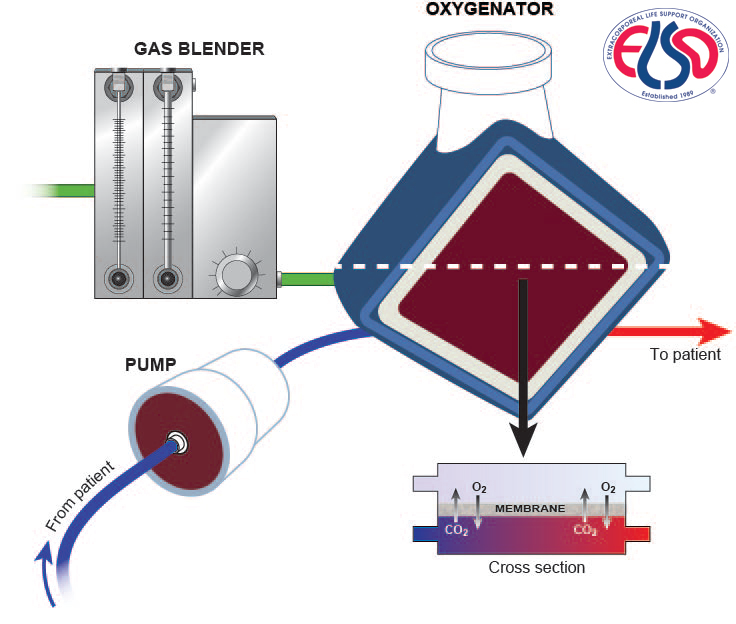
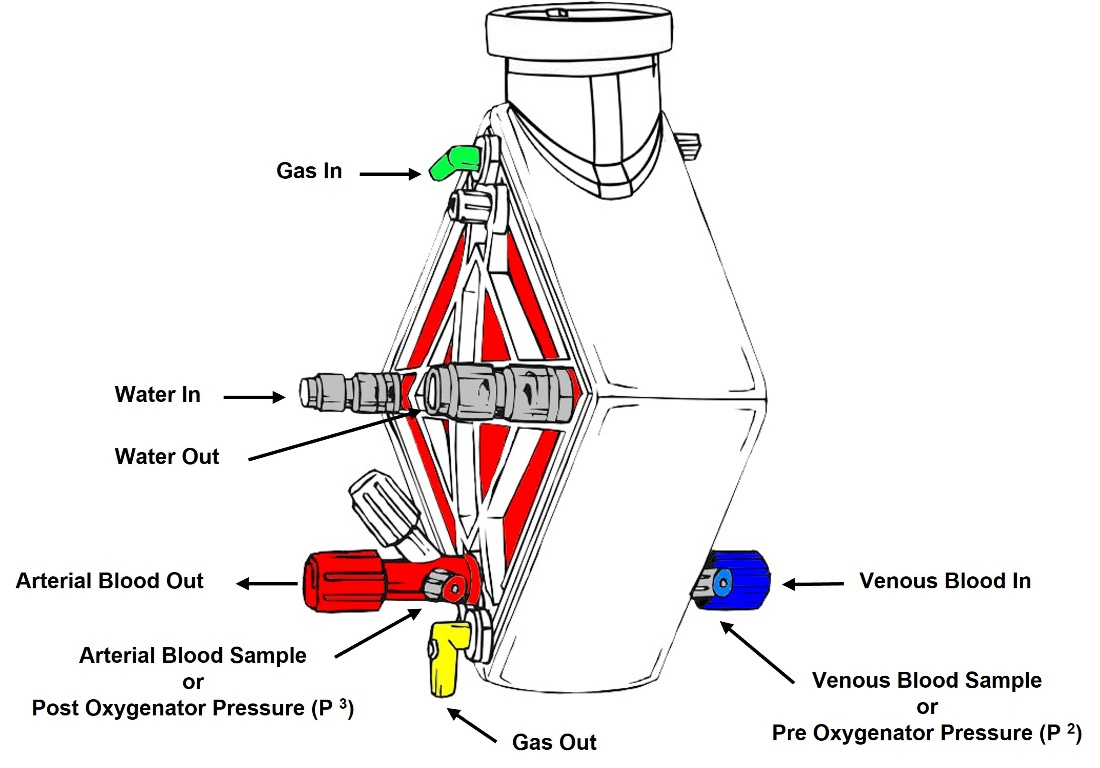
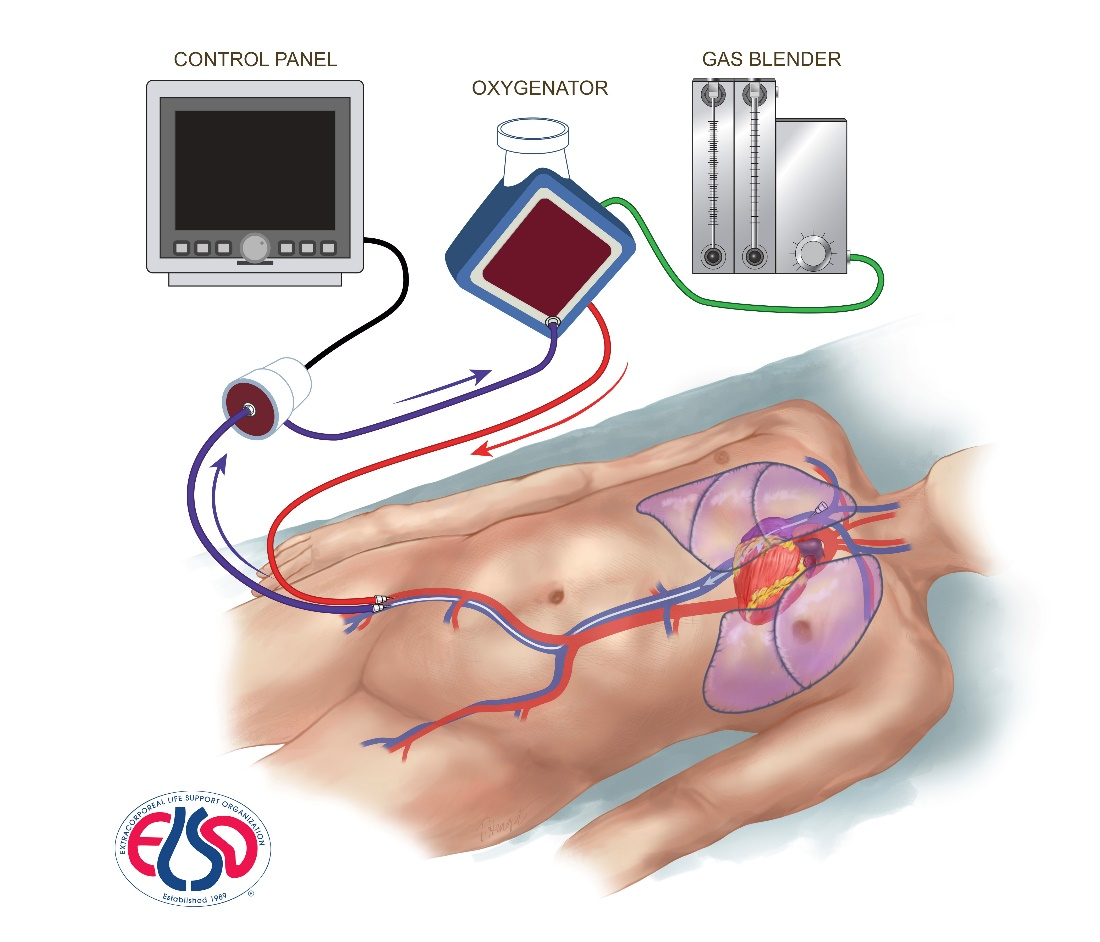
VV
Respiratory Support
VA
Cardiopulmonary Support
3-5 L/min
Typical Flow