Medical Disclaimer
- For Educational Purposes Only: This content is intended for educational reference and should not be used for clinical decision-making.
- Not a Substitute for Professional Judgment: Always consult your local protocols, institutional guidelines, and supervising physicians.
- Accuracy Not Guaranteed: While all content has been prepared to the best of my knowledge and ability, errors or omissions may exist.
- Verify Before Acting: Users are responsible for verifying information through authoritative sources before any clinical application.
AI Assistance Notice
Bedside Topline (What to Remember First)
- CRRT = slow, continuous dialysis over 24 h to support unstable ICU patients; better tolerated than intermittent hemodialysis (IHD)
- Main goals: manage volume, correct metabolic acidosis and electrolyte derangements, control uremia – while preserving hemodynamic stability
- Think in three layers: (1) Access & circuit, (2) Modality (diffusion vs convection), (3) Prescription (dose & fluid balance)
- Common modes: CVVH (convection), CVVHD (diffusion), CVVHDF (mixed), SCUF (ultrafiltration only)
- Dose in practice ≈ effluent rate 20–25 (up to 30) mL/kg/hr; more is not clearly better for mortality
- Safety bundle: strict asepsis, hourly circuit checks, careful anticoagulation, close monitoring of electrolytes, acid–base, temperature, and drug levels
Fundamentals & Terminology
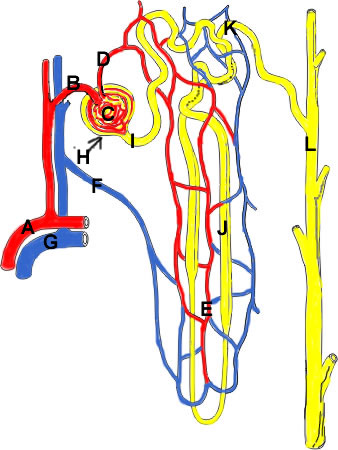
Continuous renal replacement therapy (CRRT) is any extracorporeal blood purification therapy applied continuously (~24 h/day) to replace impaired renal function in critically ill patients. It uses a hemofilter (artificial nephron) to remove water and solutes.
Key Solute Transport Mechanisms
- Diffusion: solute movement down a concentration gradient across a semipermeable membrane (dialysate on the other side). Best for small solutes (urea, K⁺)
- Convection: solvent drag – water is pulled across the membrane by transmembrane pressure and drags solutes with it. Better for middle molecules (e.g., some cytokines)
- Adsorption: some solutes adhere to the membrane surface or matrix; limited capacity and saturates over time
CRRT Modalities
Different CRRT modes use different combinations of diffusion and convection to achieve blood purification:
| Modality | Main Mechanism | Key Fluid Streams | Typical Use Case |
|---|---|---|---|
| SCUF (Slow continuous ultrafiltration) |
Ultrafiltration only | Ultrafiltrate (no dialysate or replacement) | Pure fluid removal (refractory fluid overload with relatively preserved solutes) |
| CVVH (Continuous veno-venous hemofiltration) |
Convection | Replacement fluid (pre/post-filter) + ultrafiltrate | Solute + fluid removal using convective clearance; good for uremia and volume overload |
| CVVHD (Continuous veno-venous hemodialysis) |
Diffusion | Dialysate + ultrafiltrate | Primarily small-solute clearance (e.g., hyperkalemia, uremia) with some fluid control |
| CVVHDF (Continuous veno-venous hemodiafiltration) |
Diffusion + convection | Dialysate + replacement + ultrafiltrate | Most versatile; combines excellent small-solute removal with convective middle-molecule clearance |
CRRT vs Native Kidney & Intermittent HD
Compared with the Native Kidney
- CRRT replaces only part of normal kidney function: water removal, small and some middle-solute clearance, and some acid–base control
- It does NOT replace endocrine functions (erythropoietin, vitamin D activation, renin) or fine-tuned tubular transport
- "24 h of CRRT ≈ 24 h of reduced kidney function" – it mitigates complications rather than fully normalizing physiology
CRRT vs Intermittent Hemodialysis (IHD)
| Feature | CRRT | IHD |
|---|---|---|
| Duration | 24 h/day (or near-continuous) | 2–5 h per session, several times per week |
| Fluid/solute removal rate | Slow, steady | Fast, high-volume shifts |
| Hemodynamic tolerance | Better (less hypotension) | More hypotension & osmotic shifts |
| ICU use | Preferred in unstable, ventilated patients | Often used when stable or in ESRD patients |
| Logistics | Ties to machine continuously; nursing-intensive | Short bursts; dialysis nurse-led |
Prescription – Dose, Flows & Fluid Balance
Dose of Dialysis (Small-Solute Clearance)
- In practice, CRRT dose ≈ effluent rate (dialysate + ultrafiltrate + post-filter replacement)
- Evidence suggests no mortality benefit above ~25–30 mL/kg/hr; many ICUs target 20–25 mL/kg/hr as delivered dose
- To compensate for downtime (bag changes, clots), you often prescribe slightly higher (e.g., 25–30 mL/kg/hr) to deliver ≥20 mL/kg/hr
- 70 kg patient × 25 mL/kg/hr ≈ 1750 mL/hr effluent
- 100 kg patient × 25 mL/kg/hr ≈ 2500 mL/hr effluent
- Remember: this is total effluent (dialysate + replacement + net fluid removal)
Fluid Balance Strategy
- First stabilize hemodynamics (MAP, vasopressor dose, lactate) before aggressive net negative fluid balance
- Net ultrafiltration (UFnet) = total effluent – (dialysate + replacement). Titrate UFnet to achieve desired daily balance (e.g., –500 to –2000 mL/day)
- Start with low UFnet (e.g., 0–50 mL/hr) in unstable patients; gradually increase as tolerated
- Use arterial line and echo to guide UF – watch for falling MAP, decreasing stroke volume, rising lactate, or poor organ perfusion
Anticoagulation for CRRT Circuit
Filter life and circuit patency are major determinants of effective CRRT dose. Anticoagulation is usually needed unless contraindicated.
Regional Citrate Anticoagulation (RCA)
- Mechanism: citrate chelates ionized calcium in the circuit, inhibiting coagulation; calcium is then infused systemically to normalize patient ionized Ca²⁺
- Advantages: longer filter life, lower bleeding risk than systemic heparin, especially useful in coagulopathic or post-operative patients
- Monitoring: systemic and post-filter ionized Ca²⁺, total Ca²⁺, Ca²⁺ ratio, bicarbonate/anion gap, and acid–base status
- Citrate toxicity clues: rising total:ionized calcium ratio (>2.5), metabolic acidosis or alkalosis (depending on metabolism), high anion gap, refractory hypotension; risk increased in severe liver failure and shock with poor citrate metabolism
Systemic Unfractionated Heparin
- Mechanism: systemic anticoagulation via antithrombin III; monitored with aPTT or anti-Xa
- Advantages: simple, familiar, useful when patient already requires systemic anticoagulation (e.g., PE, AF)
- Disadvantages: higher bleeding risk, filter life often shorter than with citrate; problematic in HIT
No Anticoagulation / Alternatives
- Reserved for very high bleeding risk or immediately peri-procedure; filter life is often short
- Strategies to prolong circuit life: high blood flow rates, saline flushes, minimizing stasis (avoid frequent stops), optimizing catheter position
- Alternatives like prostacyclin or regional heparin–protamine are niche and protocol-dependent
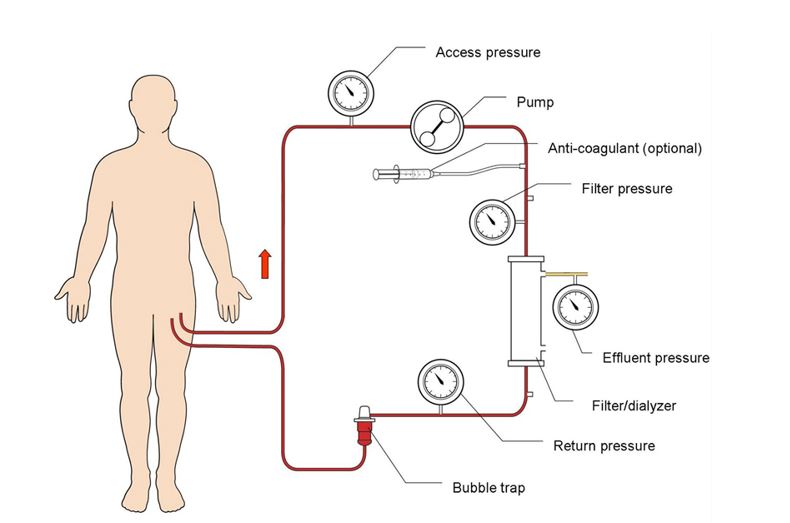
Common Alarms & Troubleshooting
| Alarm | Physiology / Cause | Quick Checks | Interventions |
|---|---|---|---|
| Access pressure low (negative) | Poor inflow from patient → catheter kinking, malposition, hypovolemia, or line occlusion | Check catheter position (neck flexion, line kink, clamps, patient position), assess volume status and CVP | Reposition patient/neck/line; flush catheter; consider volume bolus if truly hypovolemic; if persistent, consider catheter exchange |
| Return pressure high | Resistance on blood return limb → kinked tubing, clot in filter or venous chamber, high central venous pressure | Inspect line for kinks; check for visible clotting; review CVP and patient status | Correct mechanical issues; if clotting suspected, change circuit and reassess anticoagulation |
| Filter pressure high / TMP rising | Filter is clogging with clot or protein; transmembrane pressure (TMP) increases as membrane blocks | Trend TMP; look for darkening of filter, shortened filter life, frequent pressure alarms | Plan timely circuit change; optimize anticoagulation; avoid hemoconcentration (avoid aggressive UF with low blood flows) |
| Air-in-line / leak alarms | Air in circuit or leak risk; may be from empty bags, loose connections, or cracked chambers | Check all connections; ensure fluid bags not empty; inspect air detectors and drip chambers | Stop pump, clamp lines as directed, clear air per protocol; do NOT override air alarms without resolving cause |
Filter Life & P-Drop
The pressure drop (P-drop) is simply filter pressure minus return pressure. The blood pressure in the filter drops after the circuit, due to the resistance in the circuit, and from this one can estimate this resistance.
The P-drop is an important indicator of filter lifespan. An increasing P-drop signals an impending filter failure.
Complications – What Can Go Wrong
- Hemodynamic instability: excessive UF, rapid osmotic shifts, or underlying sepsis/cardiac dysfunction. Counter with slower UF, vasopressors, and careful titration
- Electrolyte derangements: hypophosphatemia, hypokalemia, hypocalcemia (especially with citrate), and sometimes hypernatremia/hyponatremia depending on fluids used
- Acid–base issues: metabolic acidosis (insufficient clearance, citrate accumulation) or metabolic alkalosis (citrate metabolism, high bicarbonate dialysate)
- Hypothermia: continuous extracorporeal circuit cools blood; may worsen coagulopathy and arrhythmias
- Bleeding: due to anticoagulation, platelet dysfunction, or line insertion; can be occult (GI, retroperitoneal)
- Catheter-related complications: infection, thrombosis, air embolism, malposition, venous stenosis
- Under-dialysis: frequent interruptions, clotted filters, low effluent prescription → inadequate solute removal and fluid burden
Bedside & Transport Pearls
- CRRT is a team sport: coordinate with nephrology/intensivist, bedside nurse, and RT when adjusting fluids, ventilator, or vasoactive drips
- Never move the patient or bed without checking line routing; avoid pulling on the dialysis catheter or filter
- During transport, strongly consider whether CRRT should run or be paused; if paused, flush lines as per protocol and document downtime
- Keep accurate input/output and weight trends; CRRT makes fluid balance look deceptively "normal" unless meticulously tracked
- Drug dosing: many critical meds (antibiotics, sedatives, anticonvulsants) are cleared by CRRT. Check local dosing guides or pharmacy for CRRT-specific doses
- For the learner: always re-check which modality is running (CVVH vs CVVHD vs CVVHDF) before interpreting flows and prescription
- Ensure battery is charged (minimum 30 min)
- Secure all lines and bags
- Brief transport team on CRRT alarms
- Have backup plan if circuit needs to be stopped
- Document downtime if CRRT paused
Quick Teaching Script (5-Step Walk-Through)
- Start with the indication: Why does this patient need CRRT (volume, K⁺, acidosis, uremia)? Why continuous vs intermittent?
- Identify the modality: Is this CVVH, CVVHD, CVVHDF, or SCUF? Which bags are dialysate vs replacement vs simply UF?
- Check the prescription: What is the effluent rate (mL/kg/hr)? What is the net UF goal (mL/hr or per day)?
- Review anticoagulation: Citrate vs heparin vs none – what are the monitoring labs and what are we watching out for (e.g., citrate toxicity, bleeding)?
- Scan for complications: pressures and alarms, electrolytes, acid–base, temperature, and catheter issues – then tie it back to how the patient looks at the bedside
Common Indications for CRRT
- Volume overload: refractory to diuretics, especially with hemodynamic instability
- Severe AKI/Uremia: BUN >100 mg/dL (or >35 mmol/L), symptoms of uremia (pericarditis, encephalopathy, bleeding)
- Refractory hyperkalemia: K⁺ >6.5 mEq/L not responsive to medical management
- Severe metabolic acidosis: pH <7.1 or bicarbonate <10 mEq/L
- Toxin removal: certain drug overdoses (lithium, metformin, salicylates – though IHD may be better for some)
- Severe electrolyte derangements: life-threatening hypernatremia, hypercalcemia, hypermagnesemia
Relative Contraindications & Cautions
- Inability to secure vascular access: coagulopathy, anatomic issues, or vascular injury
- Active uncontrolled bleeding: especially if systemic anticoagulation required
- Hemodynamic collapse: may need to stabilize first (though CRRT can help achieve this)
- Goals of care inconsistent with aggressive support: discuss with family and care team
- Severe liver failure (for citrate anticoagulation): citrate metabolism impaired, risk of toxicity
References
- London Health Sciences Centre. (2024). Principles of CRRT. Critical Care Trauma Centre, LHSC.
- Yartsev, A. (2013–2025). Continuous renal replacement therapy (CRRT) and renal intensive care chapters. Deranged Physiology. derangedphysiology.com
- Yartsev, A. (2013–2025). Definitions of CRRT terminology. Deranged Physiology.
- Yartsev, A. (2015). Anatomy of the extracorporeal dialysis circuit. Deranged Physiology. Link
- Saunders, H., & Palevsky, P. M. (2024). Continuous renal replacement therapy. In StatPearls. StatPearls Publishing.
- Prismaflex Operator's Manual (manufacturer documentation)
- KDIGO Clinical Practice Guideline for Acute Kidney Injury
- Local ICU CRRT protocols and nursing guidelines

